Practice Essentials
Arthritis encompasses a wide spectrum of disease that have the net cumulative effect of joint inflammation and subsequent destruction. Psoriatic arthritis, gout, chondrocalcinosis, and reactive arthritis may all contribute to painful joints; however, osteoarthritis and rheumatoid arthritis remain the primary focus of surgical intervention. [1]
Patients with arthritis of the hand present with pain, restricted mobility, and deformity. The underlying pathologic processes are distinguished on the basis of the history of disease onset and progression, distribution of joint involvement (monoarticular versus polyarticular), extraarticular manifestations, and review of serologic markers.
Operative treatment is indicated for the arthritic interphalangeal joint when medical management has failed to relieve the pain, when the digit deformity is interfering with hand function, or when a significant restriction of motion limits the activities of daily living. Working closely with certified hand therapists in the preoperative and postoperative periods is necessary to ensure the best outcomes.
Relatively few surgical options exist for the painful arthritic proximal interphalangeal (PIP) joint. Currently, PIP joint osteoarthritis is typically treated with arthrodesis of the index finger and silicone arthroplasties in the ulnar digits.
Anatomy of the Arthritic Interphalangeal Joint
The arthritic interphalangeal (IP) joint demonstrates fusiform joint swelling. With progression of the condition, marginal osteophytes (Bouchard nodes) become evident with progressive lateral deviation of the digits, as shown below.
 Radiograph depicting the clinical picture of a hand with fusiform swelling at the proximal interphalangeal joints. These are called Bouchard nodes.
Radiograph depicting the clinical picture of a hand with fusiform swelling at the proximal interphalangeal joints. These are called Bouchard nodes.
The proximal interphalangeal (PIP) joint is a ginglymus joint, or hinged joint, with a functional stability throughout its normal arc of flexion and extension. This bicondylar joint comprises a pair of concentric condyles that are separated by the intercondylar notch and allows a range of motion of 90-120°. The two corresponding articular surfaces of the middle phalanx are separated by a median ridge.
In contrast to the metacarpal articular head, the center of rotation of the phalangeal head remains constant throughout flexion and extension. This phalangeal joint configuration provides functional stability for lateral and rotatory forces. The oblique collateral ligaments arise from the dorsal and lateral aspect of each condyle to insert into the lateral tubercle, near the volar margin of the middle phalanx base. These collateral ligaments are 2-3 mm thick.
The volar plate consists of a distal portion of a thick fibrocartilaginous tissue that inserts into the volar lip of the middle phalanx base and is suspended by the transversely oriented accessory collateral ligaments. The proximal aspect of the volar plate is membranous and is attached to the neck of the proximal phalanx. The lateral portion of the volar plate thickens to form the volar check ligaments. See the volar view of a finger below.
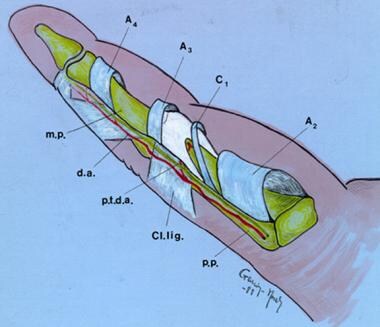 Schematic volar view of a finger. Note that between A3 and C1 is the volar plate. The lateral extension represents the restraining triangular ligaments. A2, A3, A4 = annular pulleys 2-4; C1 = cruciform pulley 1; Cl.lig. = Cleland ligament; d.a. = digital artery; m.p. = middle phalanx; p.p. = proximal phalanx; and p.t.d.a. = transverse digital artery.
Schematic volar view of a finger. Note that between A3 and C1 is the volar plate. The lateral extension represents the restraining triangular ligaments. A2, A3, A4 = annular pulleys 2-4; C1 = cruciform pulley 1; Cl.lig. = Cleland ligament; d.a. = digital artery; m.p. = middle phalanx; p.p. = proximal phalanx; and p.t.d.a. = transverse digital artery.
Additional stability is provided to the PIP joint by the extensor aponeurosis on the dorsal surface of the digit. The central slip of the extensor digitorum communis tendon attaches to the dorsal lip of the middle phalanx.
The oblique retinacular ligament arises from the side of the proximal phalanx and passes laterally into the PIP joint to join the lateral margin of the extensor band on the dorsal lateral aspect of the middle phalanx. The transverse retinacular ligament is superficial and runs dorsally from the volar surface of the capsule and flexor tendon sheath; it is attached to the lateral margin of the lateral tendon of the extensor mechanism. The Cleland ligament is dorsal to the neurovascular bundle, and the transverse Grayson ligament is volar to the neurovascular bundle, as shown below.
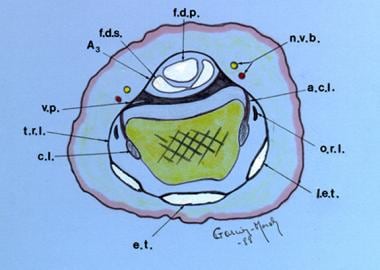 Cross-section of a finger at the proximal interphalangeal (PIP) joint level. The Cleland ligament is dorsal to the neurovascular bundle (n.v.b.), and the transverse Grayson ligament is volar to the neurovascular bundle. A3 = annular pulley 3; a.c.l. = accessory collateral ligament; c.l. = collateral ligament; e.t. = extensor tendon; f.d.p. = flexor digitorum profundus; f.d.s. = flexor digitorum superficialis; l.e.t. = lateral band; o.r.l. = oblique retinacular ligament; t.r.l. = transverse retinacular ligament; and v.p. = volar plate.
Cross-section of a finger at the proximal interphalangeal (PIP) joint level. The Cleland ligament is dorsal to the neurovascular bundle (n.v.b.), and the transverse Grayson ligament is volar to the neurovascular bundle. A3 = annular pulley 3; a.c.l. = accessory collateral ligament; c.l. = collateral ligament; e.t. = extensor tendon; f.d.p. = flexor digitorum profundus; f.d.s. = flexor digitorum superficialis; l.e.t. = lateral band; o.r.l. = oblique retinacular ligament; t.r.l. = transverse retinacular ligament; and v.p. = volar plate.
The distal interphalangeal (DIP) joint is also a hinge, or ginglymus, joint. A capsule surrounding the DIP joint is reinforced laterally by collateral ligaments that insert into the sides of the head of the middle phalanx and run in a distal and volar direction to insert into the volar lateral tubercle of the distal phalanx.
Accessory ligaments are more volar and extend from the sides of the middle phalanx head to the sides of the volar plate. The volar plate serves as an accessory insertion point for the flexor digitorum profundus. Proximally, the plate extends and is attached to the neck of the middle phalanx but does not have lateral volar extensions, as is the case with the PIP joint. [2]
Role of Surgery in the Arthritic Interphalangeal Joint
The majority of patients with interphalangeal joint arthritis respond to nonoperative interventions and thus do not need surgery. Disease-modifying antirheumatic drugs appear to have decreased dramatically the severity of rheumatic hand deformities and the frequency with which patients seek surgical consultation [3]
Operative treatment is indicated for the arthritic interphalangeal joint when medical management has failed to relieve the pain, when the digit deformity is interfering with hand function, or when a significant restriction of motion limits the activities of daily living. Working closely with certified hand therapists in the preoperative and postoperative periods is necessary to ensure the best outcomes.
The first step in any planned surgical intervention is early evaluation by a hand surgeon experienced with surgeries on the arthritic hand, to develop a treatment program that minimizes the incidence of uncorrectable late deformities. Deformity alone is not an indication for proposing surgical treatment. Rather, the surgeon ought to assess the patient’s hand impairment in work and daily activities to render recommendations as to whether surgical treatment can be beneficial. [4]
Stability considerations are as important as motion considerations, especially in the radial digits that are involved during pinching activities. During pinching, the index finger must withstand forceful contact with the thumb, especially in the lateral or key pinch. Patients with impaired index fingers pinch with the middle finger when possible, so stability of the middle finger becomes more important when the index finger is also affected.
It may also occasionally be helpful to use computed tomography to image the implant bed when planning insertion of a resurfacing arthroplasty, because it enables assessment of bone quality. [5]
Relatively few surgical options exist for the painful arthritic PIP joint. Currently, PIP joint osteoarthritis is typically treated with arthrodesis of the index finger and silicone arthroplasties in the ulnar digits.
Interphalangeal Joint Arthroplasty
Proximal interphalangeal joint (PIP) arthroplasties can be done when the patient has near-normal metacarpophalangeal joints that are reasonably well preserved. Some surgeons consider the central two digits more suitable for PIP arthroplasty because lateral stability can be supported by digits on either side. [6] Distal interphalangeal joint arthroplasty is rarely necessary, because arthroplasty of this joint results in limited motion and because function after arthrodesis is more satisfactory and predictable. [7]
A Swanson interpositional arthroplasty of the PIP joint through a dorsal approach has been recommended. [8] The volar approach, however, has better cosmetic and functional results. This approach provides an excellent exposure, which is critical given the importance of the technique with this type of procedure. However, with the volar approach, the risk of creating a swan-neck deformity exists.
A shortcoming of the Swanson implant is the sacrifice of the collateral ligaments, which makes implantation of the device in the PIP of the index or long finger undesirable. In contrast, the collateral ligaments are spared with implantation of most surface replacement arthroplasties (SRAs) of the PIP joint.
In the volar arthroplasty approach (see below), a radial- or ulnar-based Bruner incision is made, with the apex at the PIP joint flexion crease. After the skin flap is elevated, the Grayson ligaments are completely released from their origin, exposing the neurovascular bundle. The bundle is then retracted, exposing the Cleland ligaments dorsally, which are also released.
 Surgical picture of the volar approach for an arthroplasty. This image depicts the flexor tendons, retracted to the side, and the volar plate.
Surgical picture of the volar approach for an arthroplasty. This image depicts the flexor tendons, retracted to the side, and the volar plate.
The proximal and interphalangeal transverse digital arteries, which are consistently present as communicating branches from the digital arteries, are cauterized and transected, allowing full mobilization of the neurovascular structures.
The flexor tendon sheath is released by dividing the origin of the first and second cruciform pulleys and the third annular pulley at the volar plate. The volar plate is fully exposed and is released proximally and along its lateral margins from the accessory collateral ligaments, which are seen upon release of the transverse retinacular ligament from the volar capsule and tendon sheath.
The collateral ligaments are then released proximally, and the joint is opened by hyperextension, as shown below. The flexor tendons retract to one side, and the neurovascular bundles are displaced dorsally. Both articular surfaces are completely exposed in this manner.
 The proximal interphalangeal joint in hyperextension. Note the marked degenerative changes of the articular joint surface.
The proximal interphalangeal joint in hyperextension. Note the marked degenerative changes of the articular joint surface.
The medullary cavities of the bone are reamed in order to accommodate the proper size of the implant (see the images below). At this time, the authors use the recommended radiographic examination in order to assess adequate space and alignment of the digit. After the implant is inserted, it is essential for the surgeon to confirm that the digit has full range of motion and the implant is stable.
 The medullary cavities of the phalanges are prepared for placement of an implant of the proper size.
The medullary cavities of the phalanges are prepared for placement of an implant of the proper size.
 After the medullary cavities of the phalanges are prepared, an implant of the proper size is placed.
After the medullary cavities of the phalanges are prepared, an implant of the proper size is placed.
Resurfacing prosthetic procedures, with or without bone cement, have been designed for replacement of the PIP joint. Limited experience with this design has shown promise for future consideration as an alternative treatment. [9] The exposure for most surface replacement arthroplasties spares the collateral ligaments; therefore, these joint replacements are an option for the index and long fingers.
The PIP joint volar plate may be used as an interposition arthroplasty in selected individuals. Although technically demanding, this procedure may benefit patients who wish to retain motion but have contraindications to or wish not to have a nonbiological arthroplasty. Small series of patients treated with PIP joint volar plate arthroplasty have reported pain reduction and maintenance of preoperative strength and motion. [10]
Arthrodesis of the Interphalangeal Joint
Arthrodesis of the joint may be indicated for severe instability and deformity of the PIP joint or after failed arthroplasty. [11] For interphalangeal joint osteoarthritis, arthrodesis of the joint in a functional position is also an alternative treatment. Arthrodesis offers stability, durability, and little need for further procedures. [12] This option is the procedure of choice for the index finger, which is usually subjected to lateral stress during pinching activities.
Arthrodesis is indicated mainly for the index and middle fingers in patients who are young or active or when a significant loss of bone has occurred, and this procedure continues to be the best surgical treatment for the painful, unstable proximal interphalangeal (PIP) joint in the index or long finger. However, depending on the patient's needs, arthrodesis may impair or even be incompatible with satisfactory function.
Several different arthrodesis techniques for the PIP joint exist, based on the type of fixation that is used. The appropriate finger position varies for the radial to the ulnar fingers and with the assessment of the patient's particular needs. Kirschner wires (K-wires), interosseous wiring, tension band wiring, and screw fixation have been used to achieve a solid, painless arthrodesis. [13, 14, 15, 16] The rate of non-union is 0-10%.
The PIP joints should be fixed from 25° of flexion in the index finger to almost 40° in the small finger (less flexion in the radial fingers than in the ulnar fingers). The distal interphalangeal joints are fixed in 15-20° of flexion. [6]
Postoperative Care
Primary wound healing is the first goal of postoperative care. Elevation of the affected digit is important to prevent swelling. Active motion of the PIP joint usually begins on the third to seventh day, as the swelling subsides.
Following arthrodesis surgery, the PIP joint is protected in a dorsal and volar Orthoplast splint for approximately 4-6 weeks (see the image below). Motion of the metacarpophalangeal and DIP joints is allowed shortly after surgery. A hand therapist evaluates the patient to ensure adequate splinting, joint protection, and assistive devices to carry out the activities of daily living.
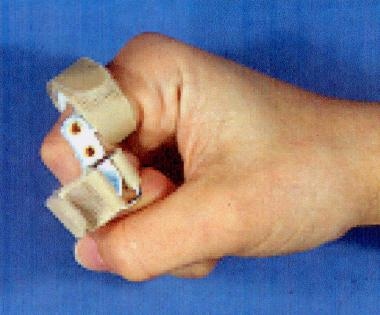 After the initial postoperative swelling subsides, the patient may wear a splint to control the lateral deviation of the digit and to encourage active range of motion.
After the initial postoperative swelling subsides, the patient may wear a splint to control the lateral deviation of the digit and to encourage active range of motion.
Outcomes
Both silicone implant arthroplasty and surface replacement arthroplasty (SRA) offer predictable motion and excellent pain relief for osteoarthritis of the interphalangeal joints. More than 90% of arthroplasties achieve a functional arc of motion of more than 40° within 6-8 weeks after surgery. The best long-term results to date have been obtained with silicone interposition arthroplasty. [17, 18] Pyrocarbon implants have yielded good pain relief and maintenance of preoperative arc of motion, but with a higher implant revision rate than other prostheses. [19, 20]
A systematic review of 40 studies reporting outcomes of implant arthroplasty for PIP with various devices and approaches found the revision rates from low to high were silicone volar (6%), silicone lateral (10%), silicone dorsal (11%), surface replacement volar (17%), and surface replacement dorsal (18%). Among the surface replacement dorsal findings, the most common types of revision surgery were revision to silicone implant (23%), arthrodesis (14%), revision with or without cement to original implant (11%), explantation of the implant (10%), amputation (4%), and other procedures (38%) [21]
The main complications of silicone devices are implant failure and cystic bone formation over time. In long-term followup, fractures have been reported in 10–30% of silicone implants. [11] A study comparing complications between 279 surface-replacing implants and 424 silicone implants found an overall complication rate of 20% for surface replacements and 11% for silicone implants. Reoperation rates were also significantly higher after surface replacement (5.5%) compared with silicone implants (0.5%). [22]
-
Radiograph depicting the clinical picture of a hand with fusiform swelling at the proximal interphalangeal joints. These are called Bouchard nodes.
-
Schematic volar view of a finger. Note that between A3 and C1 is the volar plate. The lateral extension represents the restraining triangular ligaments. A2, A3, A4 = annular pulleys 2-4; C1 = cruciform pulley 1; Cl.lig. = Cleland ligament; d.a. = digital artery; m.p. = middle phalanx; p.p. = proximal phalanx; and p.t.d.a. = transverse digital artery.
-
Cross-section of a finger at the proximal interphalangeal (PIP) joint level. The Cleland ligament is dorsal to the neurovascular bundle (n.v.b.), and the transverse Grayson ligament is volar to the neurovascular bundle. A3 = annular pulley 3; a.c.l. = accessory collateral ligament; c.l. = collateral ligament; e.t. = extensor tendon; f.d.p. = flexor digitorum profundus; f.d.s. = flexor digitorum superficialis; l.e.t. = lateral band; o.r.l. = oblique retinacular ligament; t.r.l. = transverse retinacular ligament; and v.p. = volar plate.
-
Surgical picture of the volar approach for an arthroplasty. This image depicts the flexor tendons, retracted to the side, and the volar plate.
-
The proximal interphalangeal joint in hyperextension. Note the marked degenerative changes of the articular joint surface.
-
The medullary cavities of the phalanges are prepared for placement of an implant of the proper size.
-
After the medullary cavities of the phalanges are prepared, an implant of the proper size is placed.
-
Lateral radiographic view of the finger with an implant in place.
-
Photograph depicting the degree of flexion in a hand at 10 weeks following surgery.
-
After the initial postoperative swelling subsides, the patient may wear a splint to control the lateral deviation of the digit and to encourage active range of motion.
-
After the initial postoperative swelling subsides, the patient may wear a splint to control the lateral deviation of the digit and to encourage active range of motion.









