Claesson M, Armitage WJ, Stenevi U. Corneal oedema after cataract surgery: predisposing factors and corneal graft outcome. Acta Ophthalmol. 2009 Mar. 87(2):154-9. [QxMD MEDLINE Link].
Smolin G, Thoft RA, Dohlman CH. Endothelial function. The Cornea: Scientific Foundations and Clinical Practice. 3rd ed. Lippincott William & Wilkins: 1994. 635-643.
Heckenlaible NJ, Dun C, Prescott C, Eghrari AO, Woreta F, Makary MA, et al. Predictors of Receiving Keratoplasty for Fuchs' Endothelial Corneal Dystrophy among Medicare Beneficiaries. Ophthalmology. 2023 Jan. 130 (1):28-38. [QxMD MEDLINE Link].
Stark WJ, Worthen DM, Holladay JT, et al. The FDA report on intraocular lenses. Ophthalmology. 1983 Apr. 90(4):311-17. [QxMD MEDLINE Link].
Taylor DM, Atlas BF, Romanchuk KG, Stern AL. Pseudophakic bullous keratopathy. Ophthalmology. 1983 Jan. 90(1):19-24. [QxMD MEDLINE Link].
Waring GO 3rd. The 50-year epidemic of pseudophakic corneal edema. Arch Ophthalmol. 1989 May. 107(5):657-9. [QxMD MEDLINE Link].
Shelke K, Rishi E, Rishi P. Surgical outcomes and complications of sutureless needle-guided intrascleral intraocular lens fixation combined with vitrectomy. Indian J Ophthalmol. 2021 Sep. 69 (9):2317-2320. [QxMD MEDLINE Link].
Archives of Ophthalmology. Closed-loop anterior chamber lenses. Arch Ophthalmol. 1987 Jan. 105(1):19-21. [QxMD MEDLINE Link].
Hagan JC 3rd. A clinical review of the IOLAB Azar model 91Z flexible anterior chamber intraocular lens. Ophthalmic Surg. 1987 Apr. 18(4):258-61. [QxMD MEDLINE Link].
Mamalis N, Anderson CW, Kreisler KR, Lundergan MK, Olson RJ. Changing trends in the indications for penetrating keratoplasty. Arch Ophthalmol. 1992 Oct. 110(10):1409-11. [QxMD MEDLINE Link].
Kang PC, Klintworth GK, Kim T, Carlson AN, Adelman R, Stinnett S, et al. Trends in the indications for penetrating keratoplasty, 1980-2001. Cornea. 2005 Oct. 24(7):801-3. [QxMD MEDLINE Link].
Liu E, Slomovic AR. Indications for penetrating keratoplasty in Canada, 1986-1995. Cornea. 1997 Jul. 16(4):414-9. [QxMD MEDLINE Link].
Burdon MA, McDonnell P. A survey of corneal graft practice in the United Kingdom. Eye. 1995. 9 (Pt 6 Su):6-12. [QxMD MEDLINE Link].
Williams KA, Muehlberg SM, Lewis RF, Coster DJ. How successful is corneal transplantation? A report from the Australian Corneal Graft Register. Eye. 1995. 9 (Pt 2):219-27. [QxMD MEDLINE Link].
Haamann P, Jensen OM, Schmidt P. Changing indications for penetrating keratoplasty. Acta Ophthalmol (Copenh). 1994 Aug. 72(4):443-6. [QxMD MEDLINE Link].
Dickman MM, Kruit PJ, Remeijer L, van Rooij J, Van der Lelij A, Wijdh RH, et al. A Randomized Multicenter Clinical Trial of Ultrathin Descemet Stripping Automated Endothelial Keratoplasty (DSAEK) versus DSAEK. Ophthalmology. 2016 Nov. 123 (11):2276-2284. [QxMD MEDLINE Link].
Vasiliauskaitė I, Oellerich S, Ham L, Dapena I, Baydoun L, van Dijk K, et al. Descemet Membrane Endothelial Keratoplasty: Ten-Year Graft Survival and Clinical Outcomes. Am J Ophthalmol. 2020 Sep. 217:114-120. [QxMD MEDLINE Link].
Morishige N, Chikama T, Yamada N, Takahashi N, Morita Y, Nishida T, et al. Effect of preoperative duration of stromal edema in bullous keratopathy on early visual acuity after endothelial keratoplasty. J Cataract Refract Surg. 2012 Feb. 38(2):303-8. [QxMD MEDLINE Link].
Desir J, Abramowicz M. Congenital hereditary endothelial dystrophy with progressive sensorineural deafness (Harboyan syndrome). Orphanet J Rare Dis. 2008 Oct 15. 3:28. [QxMD MEDLINE Link]. [Full Text].
Srinivasan S, Skarmoutsos P, O'Donnell C, Kaye SB. Localized bullous keratopathy secondary to posterior polymorphous dystrophy. Clin Experiment Ophthalmol. 2008 Nov. 36(8):800-1. [QxMD MEDLINE Link].
Dick HB, Kohnen T, Jacobi FK, Jacobi KW. Long-term endothelial cell loss following phacoemulsification through a temporal clear corneal incision. J Cataract Refract Surg. 1996 Jan-Feb. 22(1):63-71. [QxMD MEDLINE Link].
Hayashi K, Hayashi H, Nakao F, Hayashi F. Risk factors for corneal endothelial injury during phacoemulsification. J Cataract Refract Surg. 1996 Oct. 22(8):1079-84. [QxMD MEDLINE Link].
Werblin TP. Long-term endothelial cell loss following phacoemulsification: model for evaluating endothelial damage after intraocular surgery. Refract Corneal Surg. 1993 Jan-Feb. 9(1):29-35. [QxMD MEDLINE Link].
Hoffer KJ. Cell loss with superior and temporal incisions. J Cataract Refract Surg. 1994 May. 20(3):368. [QxMD MEDLINE Link].
Lundberg B, Jonsson M, Behndig A. Postoperative corneal swelling correlates strongly to corneal endothelial cell loss after phacoemulsification cataract surgery. Am J Ophthalmol. 2005 Jun. 139(6):1035-41. [QxMD MEDLINE Link].
Morikubo S, Takamura Y, Kubo E, Tsuzuki S, Akagi Y. Corneal changes after small-incision cataract surgery in patients with diabetes mellitus. Arch Ophthalmol. 2004 Jul. 122 (7):966-9. [QxMD MEDLINE Link].
Richard J, Hoffart L, Chavane F, Ridings B, Conrath J. Corneal endothelial cell loss after cataract extraction by using ultrasound phacoemulsification versus a fluid-based system. Cornea. 2008 Jan. 27(1):17-21. [QxMD MEDLINE Link].
Storr-Paulsen A, Norregaard JC, Ahmed S, Storr-Paulsen T, Pedersen TH. Endothelial cell damage after cataract surgery: divide-and-conquer versus phaco-chop technique. J Cataract Refract Surg. 2008 Jun. 34(6):996-1000. [QxMD MEDLINE Link].
Park J, Yum HR, Kim MS, Harrison AR, Kim EC. Comparison of phaco-chop, divide-and-conquer, and stop-and-chop phaco techniques in microincision coaxial cataract surgery. J Cataract Refract Surg. 2013 Oct. 39(10):1463-9. [QxMD MEDLINE Link].
Koch DD, Liu JF, Glasser DB, Merin LM, Haft E. A comparison of corneal endothelial changes after use of Healon or Viscoat during phacoemulsification. Am J Ophthalmol. 1993 Feb 15. 115(2):188-201. [QxMD MEDLINE Link].
Zavodni ZJ, Meyer JJ, Kim T. Clinical Features and Outcomes of Retained Lens Fragments in the Anterior Chamber After Phacoemulsification. Am J Ophthalmol. 2015 Dec. 160 (6):1171-1175.e1. [QxMD MEDLINE Link].
Moshirfar M, Lewis AL, Ellis JH, McCabe SE, Ronquillo YC, Hoopes PC Sr. Anterior Chamber Retained Lens Fragments After Cataract Surgery: A Case Series and Narrative Review. Clin Ophthalmol. 2021. 15:2625-2633. [QxMD MEDLINE Link].
Lugo M, Cohen EJ, Eagle RC Jr, Parker AV, Laibson PR, Arentsen JJ. The incidence of preoperative endothelial dystrophy in pseudophakic bullous keratopathy. Ophthalmic Surg. 1988 Jan. 19(1):16-9. [QxMD MEDLINE Link].
Adamis AP, Filatov V, Tripathi BJ, Tripathi RC. Fuchs' endothelial dystrophy of the cornea. Surv Ophthalmol. 1993 Sep-Oct. 38(2):149-68. [QxMD MEDLINE Link].
Arnalich-Montiel F, de-Arriba-Palomero P, Muriel A, Mingo-Botín D. A Risk Prediction Model for Endothelial Keratoplasty After Uncomplicated Cataract Surgery in Fuchs Endothelial Corneal Dystrophy. Am J Ophthalmol. 2021 Nov. 231:70-78. [QxMD MEDLINE Link].
Tey KY, Tan SY, Ting DSJ, Mehta JS, Ang M. Effects of Combined Cataract Surgery on Outcomes of Descemet's Membrane Endothelial Keratoplasty: A Systematic Review and Meta-Analysis. Front Med (Lausanne). 2022. 9:857200. [QxMD MEDLINE Link].
Edelhauser HF, Van Horn DL, Hyndiuk RA, Schultz RO. Intraocular irrigating solutions. Their effect on the corneal endothelium. Arch Ophthalmol. 1975 Aug. 93(8):648-57. [QxMD MEDLINE Link].
Edelhauser HF, Gonnering R, Van Horn DL. Intraocular irrigating solutions. A comparative study of BSS Plus and lactated Ringer's solution. Arch Ophthalmol. 1978 Mar. 96(3):516-20. [QxMD MEDLINE Link].
Koenig SB, Schultz RO. Penetrating keratoplasty for pseudophakic bullous keratopathy after extracapsular cataract extraction. Am J Ophthalmol. 1988 Apr 15. 105(4):348-53. [QxMD MEDLINE Link].
Bowen RC, Zhou AX, Bondalapati S, Lawyer TW, Snow KB, Evans PR, et al. Comparative analysis of the safety and efficacy of intracameral cefuroxime, moxifloxacin and vancomycin at the end of cataract surgery: a meta-analysis. Br J Ophthalmol. 2018 Sep. 102 (9):1268-1276. [QxMD MEDLINE Link].
Mamalis N, Edelhauser HF, Dawson DG, Chew J, LeBoyer RM, Werner L. Toxic anterior segment syndrome. J Cataract Refract Surg. 2006 Feb. 32(2):324-33. [QxMD MEDLINE Link].
Kang HM, Park JW, Chung EJ. A retained lens fragment induced anterior uveitis and corneal edema 15 years after cataract surgery. Korean J Ophthalmol. 2011 Feb. 25(1):60-2. [QxMD MEDLINE Link]. [Full Text].
Chu MJ, Song M, Palmares T, Song A, Song J. Rhopressa-induced corneal edema: a case report. J Med Case Rep. 2021 Apr 2. 15 (1):182. [QxMD MEDLINE Link].
LoBue SA, Moustafa GA, Vu A, Amin M, Nguyen T, Goyal H. Transient Reticular Cystic Corneal Epithelial Edema With Topical Netarsudil: A Case Series and Review. Cornea. 2021 Aug 1. 40 (8):1048-1054. [QxMD MEDLINE Link].
Tran JA, Jurkunas UV, Yin J, Davies EC, Sola-Del Valle DA, Chen TC, et al. Netarsudil-associated reticular corneal epithelial edema. Am J Ophthalmol Case Rep. 2022 Mar. 25:101287. [QxMD MEDLINE Link].
Homer PI, Peyman GA, Sugar J. Automated vitrectomy in eyes with vitreocorneal touch associated with corneal dysfunction. Am J Ophthalmol. 1980 Apr. 89(4):500-6. [QxMD MEDLINE Link].
McCarey BE, Edelhauser HF, Lynn MJ. Review of corneal endothelial specular microscopy for FDA clinical trials of refractive procedures, surgical devices, and new intraocular drugs and solutions. Cornea. 2008 Jan. 27 (1):1-16. [QxMD MEDLINE Link].
Moshirfar M, Duong A, Ronquillo Y. Corneal Imaging. 2022 Jan. [QxMD MEDLINE Link]. [Full Text].
Li YJ, Kim HJ, Joo CK. Early changes in corneal edema following torsional phacoemulsification using anterior segment optical coherence tomography and Scheimpflug photography. Jpn J Ophthalmol. 2011 May. 55 (3):196-204. [QxMD MEDLINE Link].
Liu GJ, Okisaka S, Mizukawa A, Momose A. Histopathological study of pseudophakic bullous keratopathy developing after anterior chamber of iris-supported intraocular lens implantation. Jpn J Ophthalmol. 1993. 37(4):414-25. [QxMD MEDLINE Link].
Melles GR. Posterior lamellar keratoplasty: DLEK to DSEK to DMEK. Cornea. 2006 Sep. 25(8):879-81. [QxMD MEDLINE Link].
Zander DB, Böhringer D, Fritz M, Grewing V, Maier PC, Lapp T, et al. Hyperosmolar Eye Drops for Diurnal Corneal Edema in Fuchs' Endothelial Dystrophy: A Double-Masked, Randomized Controlled Trial. Ophthalmology. 2021 Nov. 128 (11):1527-1533. [QxMD MEDLINE Link].
Cormier G, Brunette I, Boisjoly HM, LeFrançois M, Shi ZH, Guertin MC. Anterior stromal punctures for bullous keratopathy. Arch Ophthalmol. 1996 Jun. 114(6):654-8. [QxMD MEDLINE Link].
Arora R, Manudhane A, Saran RK, Goyal J, Goyal G, Gupta D. Role of corneal collagen cross-linking in pseudophakic bullous keratopathy: a clinicopathological study. Ophthalmology. 2013 Dec. 120 (12):2413-2418. [QxMD MEDLINE Link].
Ghanem RC, Santhiago MR, Berti TB, Thomaz S, Netto MV. Collagen crosslinking with riboflavin and ultraviolet-A in eyes with pseudophakic bullous keratopathy. J Cataract Refract Surg. 2010 Feb. 36 (2):273-6. [QxMD MEDLINE Link].
Sharma N, Roy S, Maharana PK, Sehra SV, Sinha R, Tandon R, et al. Outcomes of corneal collagen crosslinking in pseudophakic bullous keratopathy. Cornea. 2014 Mar. 33 (3):243-6. [QxMD MEDLINE Link].
Brightbill FS. Penetrating keratoplasty for pseudophakic bullous keratopathy. Corneal Surgery: Theory, Technique and Tissue. Mosby Inc; 1992. 151-163.
Brightbill FS. Lens replacement in pseudophakic bullous keratopathy: anterior chamber intraocular lenses. Corneal Surgery: Theory, Technique and Tissue. 2nd ed. Mosby Inc; 1992. 163-7.
Brightbill FS. Posterior chamber intraocular lenses-scleral fixated. Corneal Surgery: Theory, Technique and Tissue. 2nd ed. Mosby Inc; 1992. 171-176.
Donaldson KE, Gorscak JJ, Budenz DL, Feuer WJ, Benz MS, Forster RK. Anterior chamber and sutured posterior chamber intraocular lenses in eyes with poor capsular support. J Cataract Refract Surg. 2005 May. 31(5):903-9. [QxMD MEDLINE Link].
Pande M, Noble BA. The role of intraocular lens exchange in the management of major implant-related complications. Eye. 1993. 7 (Pt 1):34-9. [QxMD MEDLINE Link].
Agarwal A, Jacob S, Kumar DA, Agarwal A, Narasimhan S, Agarwal A. Handshake technique for glued intrascleral haptic fixation of a posterior chamber intraocular lens. J Cataract Refract Surg. 2013 Mar. 39(3):317-22. [QxMD MEDLINE Link].
Yamane S, Sato S, Maruyama-Inoue M, Kadonosono K. Flanged Intrascleral Intraocular Lens Fixation with Double-Needle Technique. Ophthalmology. 2017 Aug. 124 (8):1136-1142. [QxMD MEDLINE Link].
Weene LE. Flexible open-loop anterior chamber intraocular lens implants. Ophthalmology. 1993 Nov. 100(11):1636-9. [QxMD MEDLINE Link].
Zaidman GW, Goldman S. A prospective study on the implantation of anterior chamber intraocular lenses during keratoplasty for pseudophakic and aphakic bullous keratopathy. Ophthalmology. 1990 Jun. 97(6):757-62. [QxMD MEDLINE Link].
Donnenfeld ED, Ingraham HJ, Perry HD, Russell S, Foulks G. Soemmering's ring support for posterior chamber intraocular lens implantation during penetrating keratoplasty. Changing trends in bullous keratopathy. Ophthalmology. 1992 Aug. 99(8):1229-33. [QxMD MEDLINE Link].
Kristianslund O, Sandvik GF, Drolsum L. Long-Term Suture Breakage After Scleral Fixation of a Modified Capsular Tension Ring with Polypropylene 10-0 Suture. Clin Ophthalmol. 2021. 15:2473-2479. [QxMD MEDLINE Link].
Lau THA, Garg A, Popovic MM, Kertes PJ, Muni RH. Scleral-fixated and iris-fixated intraocular lens implantation or fixation:meta-analysis. J Cataract Refract Surg. 2022 Dec 1. 48 (12):1462-1468. [QxMD MEDLINE Link].
Terry MA, Saad HA, Shamie N, Chen ES, Phillips PM, Friend DJ, et al. Endothelial keratoplasty: the influence of insertion techniques and incision size on donor endothelial survival. Cornea. 2009 Jan. 28 (1):24-31. [QxMD MEDLINE Link].
Wandling GR Jr, Rauen MP, Goins KM, Kitzmann AS, Sutphin JE, Kwon YH, et al. Glaucoma therapy escalation in eyes with pseudophakic corneal edema after penetrating keratoplasty and Descemet's stripping automated endothelial keratoplasty. Int Ophthalmol. 2012 Jan 13. [QxMD MEDLINE Link].
Price FW Jr, Price MO. Evolution of endothelial keratoplasty. Cornea. 2013 Nov. 32 Suppl 1:S28-32. [QxMD MEDLINE Link].
Tenkman LR, Price FW, Price MO. Descemet membrane endothelial keratoplasty donor preparation: navigating challenges and improving efficiency. Cornea. 2014 Mar. 33(3):319-25. [QxMD MEDLINE Link].
Rose-Nussbaumer J, Lin CC, Austin A, Liu Z, Clover J, McLeod SD, et al. Descemet Endothelial Thickness Comparison Trial: Two-Year Results from a Randomized Trial Comparing Ultrathin Descemet Stripping Automated Endothelial Keratoplasty with Descemet Membrane Endothelial Keratoplasty. Ophthalmology. 2021 Aug. 128 (8):1238-1240. [QxMD MEDLINE Link].
Anshu A, Price MO, Price FW Jr. Risk of corneal transplant rejection significantly reduced with Descemet's membrane endothelial keratoplasty. Ophthalmology. 2012 Mar. 119 (3):536-40. [QxMD MEDLINE Link].
Woo JH, Ang M, Htoon HM, Tan D. Descemet Membrane Endothelial Keratoplasty Versus Descemet Stripping Automated Endothelial Keratoplasty and Penetrating Keratoplasty. Am J Ophthalmol. 2019 Nov. 207:288-303. [QxMD MEDLINE Link].
Morikubo S, Takamura Y, Kubo E, Tsuzuki S, Akagi Y. Corneal changes after small-incision cataract surgery in patients with diabetes mellitus. Arch Ophthalmol. 2004 Jul. 122(7):966-9. [QxMD MEDLINE Link].
Abell RG, Kerr NM, Howie AR, Mustaffa Kamal MA, Allen PL, Vote BJ. Effect of femtosecond laser-assisted cataract surgery on the corneal endothelium. J Cataract Refract Surg. 2014 Nov. 40 (11):1777-83. [QxMD MEDLINE Link].
Olson RJ, Kolodner H, Riddle P, Escapini H Jr. Commonly used intraocular medications and the corneal endothelium. Arch Ophthalmol. 1980 Dec. 98(12):2224-6. [QxMD MEDLINE Link].
Bleckmann H, Kaczmarek U. Functional results of posterior chamber lens implantation with scleral fixation. J Cataract Refract Surg. 1994 May. 20(3):321-6. [QxMD MEDLINE Link].
Terry MA, Ousley PJ. Replacing the endothelium without corneal surface incisions or sutures: the first United States clinical series using the deep lamellar endothelial keratoplasty procedure. Ophthalmology. 2003 Apr. 110(4):755-64; discussion 764. [QxMD MEDLINE Link].
Gorovoy MS. Descemet-stripping automated endothelial keratoplasty. Cornea. 2006 Sep. 25(8):886-9. [QxMD MEDLINE Link].
Price MO, Price FW Jr. Descemet's stripping with endothelial keratoplasty: comparative outcomes with microkeratome-dissected and manually dissected donor tissue. Ophthalmology. 2006 Nov. 113(11):1936-42. [QxMD MEDLINE Link].
Price MO, Price FW. Descemet's stripping endothelial keratoplasty. Curr Opin Ophthalmol. 2007 Jul. 18(4):290-4. [QxMD MEDLINE Link].
Terry MA, Saad HA, Shamie N, et al. Endothelial keratoplasty: the influence of insertion techniques and incision size on donor endothelial survival. Cornea. 2009 Jan. 28(1):24-31. [QxMD MEDLINE Link].
Smolin G, Thoft RA, Dohlman CH. Corneal dystrophies and degenerations. The Cornea: Scientific Foundations and Clinical Practice. 3rd ed. Lippincott William & Wilkins: 1994. 520-522.
Gothard TW, Hardten DR, Lane SS, Doughman DJ, Krachmer JH, Holland EJ. Clinical findings in Brown-McLean syndrome. Am J Ophthalmol. 1993 Jun 15. 115(6):729-37. [QxMD MEDLINE Link].
Wandling GR Jr, Rauen MP, Goins KM, Kitzmann AS, Sutphin JE, Kwon YH, et al. Glaucoma therapy escalation in eyes with pseudophakic corneal edema after penetrating keratoplasty and Descemet's stripping automated endothelial keratoplasty. Int Ophthalmol. 2012 Feb. 32 (1):9-14. [QxMD MEDLINE Link].
Price FW Jr, Price MO. Evolution of endothelial keratoplasty. Cornea. 2013 Nov. 32 Suppl 1:S28-32. [QxMD MEDLINE Link].
Tenkman LR, Price FW, Price MO. Descemet membrane endothelial keratoplasty donor preparation: navigating challenges and improving efficiency. Cornea. 2014 Mar. 33 (3):319-25. [QxMD MEDLINE Link].
Price MO, Price FW Jr. Descemet's stripping with endothelial keratoplasty: comparative outcomes with microkeratome-dissected and manually dissected donor tissue. Ophthalmology. 2006 Nov. 113 (11):1936-42. [QxMD MEDLINE Link].
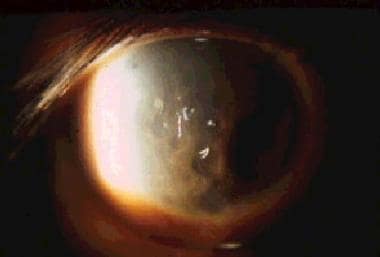 Pseudophakic bullous keratopathy. Large multiple bullae, such as depicted here, are associated with moderate to severe pain and discomfort.
Pseudophakic bullous keratopathy. Large multiple bullae, such as depicted here, are associated with moderate to severe pain and discomfort.
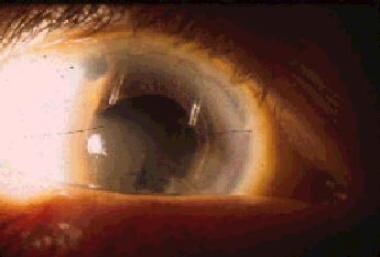 Pseudophakic bullous keratopathy. This patient has a closed-loop anterior chamber intraocular lens (Leiske model).
Pseudophakic bullous keratopathy. This patient has a closed-loop anterior chamber intraocular lens (Leiske model).


