Practice Essentials
The glenohumeral joint normally functions through a wide range of motions in a smooth, congruent fashion. When the articular surfaces of the humeral head or the glenoid are damaged, the smooth, fluid motion is compromised, and arthritis commonly is the result. The anteroposterior anatomy of the glenohumeral joint is demonstrated in the image below.
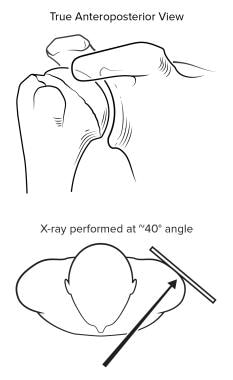 The diagnosis of shoulder osteoarthritis (OA) is made on the basis of the history, physical examination, and standard radiographs. A true anteroposterior (AP) view is necessary to gauge the degree of joint space narrowing.
The diagnosis of shoulder osteoarthritis (OA) is made on the basis of the history, physical examination, and standard radiographs. A true anteroposterior (AP) view is necessary to gauge the degree of joint space narrowing.
Glenohumeral arthritis impacts approximately 32% of individuals over the age of 60. [1] The number of patients presenting with symptoms attributable to glenohumeral arthritis has increased tremendously over the past decade. The reasons for this are multifactorial, including the aging of the population and an increased awareness that, like the hip and knee, the shoulder is not immune to developing arthritis.
A cohort study of 596,874 patients across six body mass index (BMI) cohorts found that, compared with persons with a normal BMI, those with a BMI over 24 kg/m2 were at increased risk of developing glenohumeral osteoarthritis, and those with a BMI less than 19 were at significantly reduced risk. Individuals with glenohumeral osteoarthritis and a BMI over 30 had increased odds of undergoing arthroplasty. [2]
The American College of Radiology (ACR) has published appropriateness criteria for imaging in patients with chronic shoulder pain. [3] Radiographs of the shoulder are the most appropriate initial imaging study; ultrasound (US) of the shoulder may also be appropriate. For subsequent imaging of the shoulder, procedures that are usually appropriate depend on the findings in the initial study, as follows:
-
Normal or inconclusive findings, in a patient with clinically suspected rotator cuff disorder or subacromial subdeltoid bursitis (no prior surgery): US, magnetic resonance (MR) arthrography, or magnetic resonance imaging (MRI)
-
Calcific tendinopathy or calcific bursitis: Image-guided injection of anesthetic +/- corticosteroid into the shoulder or surrounding structures; US, MR arthrography, or MRI without intravenous (IV) contrast may be appropriate
-
Normal or inconclusive findings, in a patient with clinically suspected labral pathology or shoulder instability: MR arthrography or MRI without IV contrast; computed tomography (CT) without IV contrast or CT arthrography may be appropriate
-
Normal or inconclusive findings, in a patient with clinically suspected adhesive capsulitis: Image-guided injection of anesthetic +/- corticosteroid into the shoulder or surrounding structures, or MRI without IV contrast; MR arthrography may be appropriate; there is disagreement over the appropriateness of US
-
Normal or inconclusive findings, in a patient with clinically suspected biceps tendon abnormality: US, image-guided injection of anesthetic +/- corticosteroid into the shoulder or surrounding structures, MR arthrography, or MRI without IV contrast; CT arthrography may be appropriate
-
Osteoarthritis: MRI without IV contrast; image-guided injection of anesthetic +/- corticosteroid into the shoulder or surrounding structures, MR arthrography, CT without IV contrast, or CT arthrography may be appropriate
-
Normal or inconclusive findings, in a patient with a past history of rotator cuff repair and clinically suspected rotator cuff disorders or subacromial subdeltoid bursitis: US, MR arthrography, MRI without IV contrast, or CT arthrography; image-guided injection of anesthetic +/- corticosteroid into the shoulder or surrounding structures may be appropriate
Shoulder arthroplasty
The field of arthroplasty (ie, replacing a worn joint with an artificial one) has grown tremendously since the late 20th century. Although the first shoulder replacement was performed in 1893, the field of shoulder arthroplasty did not come into the mainstream until the 1970s, lagging behind hip and knee arthroplasty.
Many shoulder arthroplasty designs have been tested over the years, and various strengths and weaknesses have been noted. Two terms require definition at this point. Hemiarthroplasty, as the name suggests, describes replacing one half of the joint, the humeral side, with an artificial component, thus allowing the prosthesis to articulate with the native glenoid. Total shoulder arthroplasty involves prosthetic replacement of the humeral head and the glenoid.
The different implants introduced over the years can be classified into 3 general types: anatomic, semiconstrained, and constrained. Anatomic designs sought to recreate the normal anatomic relationships and contours of the humeral head and glenoid. Due to these design parameters, anatomic implants had a large amount of rotational movement and were termed unconstrained. Early anatomic implants had a significant rate of loosening, in part due to the materials available and the surgical techniques used at the time.
Semiconstrained implants sought to increase the stability lacking in the early anatomic prostheses by employing a hooded glenoid to help capture the humeral head. Fully constrained prostheses were ball-in-socket implants. These implants initially provided good stability but were difficult to place. Fully constrained implants had high rates of breakage and loosening. Modularity, which was an attempt to accommodate for anatomic variations, was introduced in the 1980s.
Another important design parameter concerned the type of fixation, with cemented versus uncemented options. Cemented and uncemented humeral implants showed good long-term results. However, cementless glenoid components yielded high rates of failure.
Current total shoulder arthroplasty designs employ a nonconstrained design, usually consisting of a polyethylene glenoid component and a stemmed metallic humeral head component. The humeral component can be either a cemented or uncemented type, with the glenoid being cemented into place. Restoring normal kinematics and soft-tissue tension is of utmost importance for long-term success.
Shoulder Anatomy
The four basic characteristics essential to normal shoulder function are motion, stability, strength, and smoothness.
Motion
By virtue of its anatomy, the shoulder joint is the most mobile joint in the body. Several factors influence this mobility.
First, capsular laxity plays a key role. Capsular tissue surrounds the entire joint, and its cells lubricate the joint. The capsule normally is lax through most of the functional range of motion (ROM), but as the joint approaches the end of its normal arc, the capsule and its ligaments become tense, thus serving as checkreins to further rotation. If the capsule loses its normal laxity, either through a disease process or iatrogenically, these structures may become tight during normal functional ROM, thus leading to a stiff shoulder.
Obligate translation is a term used to describe translational movement of the humeral head at the end range of motion (ROM). Obligate translation occurs as a result of capsular tension and is defined by movement of the humeral head in a direction opposite that of the tight capsule.
Anterior translations usually occur during terminal flexion and cross-body adduction, while posterior translation occurs at terminal extension and external rotation. If asymmetrical capsular contracture is present, obligate translation may occur prematurely, resulting in chondral shear and potential articular degeneration.
Stability
The lack of anatomic restraint between the humeral head and the glenoid allows tremendous motion to occur at this joint, but it also confers an inherent instability. This inherent lack of stability is combated in several ways. The requisites for stability include an anatomically oriented humeral head, a sufficiently extensive humeral articular surface area, an anatomically oriented glenoid, a glenoid cavity with sufficiently large effective arcs, and control of net humeral reaction force.
The orientation of the humeral head with respect to the shaft is defined by the angle formed between a line drawn through the center of the anatomic neck and a line drawn through the center of the humeral head. The normal head-shaft angle is about 130°, with about 30° of retroversion. An anatomic variant with significant deviation from these angles can lead to inherent instability. The articular surface area of the humeral head is larger than that of the glenoid, thus allowing for large normal ROM.
Glenoid version, the angle formed between the center of the glenoid and the scapular body, is critically important for stability. In osteoarthritis (OA), posterior glenoid wear is predominant, leading to increased retroversion of the glenoid and predisposing to posterior instability. Coupled to these concepts of glenoid orientation are glenoid concavity and the possible effective arcs. The arc is defined by the maximal angle of motion possible before dislocation occurs. With asymmetrical glenoid rim wear, less effective arcs are possible.
The net humeral joint reaction force is determined by combining the magnitude and direction of all of the muscle forces acting across the shoulder, including those of the rotator cuff and the deltoid muscle groups. Neural control affects the magnitude of different muscle-group forces and, therefore, is the mechanism by which the direction of the resulting force is modulated. Tendon ruptures or selective weakness of a muscle group can lead to eccentric loading of the joint and accelerated wear or loosening of a prosthesis.
Strength
Although strength is inherently coupled with stability, it nevertheless should be considered separately. The requisites for good shoulder function are a functional deltoid and rotator cuff. Muscles are functional when they have sufficient power and proper alignment. Contractions may not affect power, but they may affect excursion of the tendon and, thus, the movement of the arm.
Smoothness
Normal articular glide is required for the shoulder to reach the entire effective arc. Synovial fluid provides a thin layer of lubrication between the articular surfaces. The relatively smooth articular surface, combined with the synovial fluid, allows smooth, fluid motion with very little resistance. However, if the surfaces become rough, as with loss of articular cartilage, the coefficient of friction and relative resistance between 2 gliding objects greatly increases. In addition, with increased resistance, the amount of wear increases tremendously.
Shoulder Arthritides
Glenohumeral arthritis may result from degeneration, trauma (including iatrogenic), inflammation, infection, or neuropathy.
Degeneration-related arthritis
The disease process in OA of the shoulder parallels that of other joints. Progressive, asymmetrical narrowing of the joint space and fibrillation of the articular cartilage occur. Subchondral sclerosis and osteophyte formation follow. In later stages, complete loss of articular cartilage occurs, with bony destruction following.
Posttrauma arthritis
Arthritis that occurs posttrauma is also referred to as secondary degenerative arthritis. Secondary arthritis exists when a specific cause can be identified. Causative agents include trauma, fracture, and instability. Fracture can result from trauma or can occur during surgery (eg, during glenoid realignment osteotomy). Depending on the exact etiology, posttraumatic arthritis is characterized by osseous deformities and asymmetrical soft-tissue contractures.
According to several published studies, approximately 1 in 10 patients with untreated shoulder instability develop destructive changes within 10 years; this condition is known as dislocation arthropathy. However, in one study, 26.3% of patients undergoing surgical stabilization for recurrent instability already demonstrated early signs of osteoarthritis (OA) on CT scan at the time of surgery. Thus, even though surgical stabilization is often recommended for young patients with shoulder instability, OA may continue to develop. Evidence suggests that the risk factors for OA include the number of dislocations/subluxations, age at time of first dislocation, age at time of surgery, limitations in external humeral rotation, and rotator cuff involvement. [4]
Inflammatory arthritides
Inflammatory arthritides make up the second largest category of glenohumeral arthritis. The shoulder commonly is affected in individuals with inflammatory arthritides. The prototypical disease in this category is rheumatoid arthritis (RA). In one study, 91% of patients with RA reported shoulder pain and functional limitations.
Other inflammatory diseases that may affect the shoulder include systemic lupus erythematosus (SLE), gout, pseudogout, ankylosing spondylitis, and psoriatic arthritis. In all of these diseases, including RA, the pathologic processes are similar. The initial stage of RA of the shoulder involves an intense synovitis. Inflammatory mediators released by this hypertrophic synovium, such as collagenases and proteases, lead to direct joint destruction. The inflamed synovium and mediators cause a painful distension of the joint capsule, leading the patient to splint the shoulder and avoid the extremes of motion.
Without full motion, the humeral head undergoes little obligate translation, which leads to relatively central maintenance of the head. The humeral head places pressure on the already weakened central glenoid articular cartilage, leading to erosions in the glenoid center. The thickened, inflamed capsule and synovium, coupled with the voluntary splinting of the arm, leads to circumferential tightening of the joint, which then leads to fixed restriction of motion.
Large, marginal erosions may be present, often altering normal humeral anatomy. In many patients, the humeral head ascends in relation to the glenoid. This is thought to be due to loss of the superomedial articular surface and not due to a full-thickness rotator cuff tear. Indeed, in patients undergoing arthroplasty for RA, only 10-40% had full-thickness rotator cuff tears at the time of surgery. Tears in the rotator cuff usually occur from direct invasion and destruction by the inflamed synovium, as well as from impingement erosion secondary to a superiorly translated humeral head.
For the remainder of this article, RA is discussed here as the prototype of inflammatory arthritides. The management principles in RA are the same as in the other inflammatory processes.
Cuff tear arthropathy
This shoulder-specific arthritis occurs in persons, usually elderly, who have a long-standing, massive rotator cuff tear. Several theories as to its etiology exist.
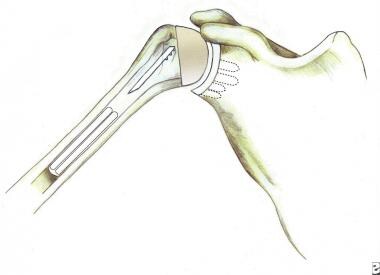
Neer hypothesized that loss of the normal head-depressor function of the rotator cuff leads to progressive superior instability. Over time, the humeral head articulates with the coracoacromial arch, as seen in the image below. The articular cartilage superiorly is subjected to pressure and erodes secondary to abrasion.
 Radiograph demonstrating superior migration of the humeral head. This is seen in the setting of a long-standing massive rotator cuff tear where the normal function of the rotator cuff acting as a humeral head depressor has been lost.
Radiograph demonstrating superior migration of the humeral head. This is seen in the setting of a long-standing massive rotator cuff tear where the normal function of the rotator cuff acting as a humeral head depressor has been lost.
Neer also suggested that loss of the rotator cuff might lead to escape of the glenohumeral synovial fluid, resulting in a nutritional loss to the articular cartilage, with subsequent degeneration. Finally, some rheumatology literature describes this condition as occurring secondary to hydroxyapatite crystal deposition disease, the Milwaukee shoulder.
Capsulorraphy arthropathy
Capsulorraphy arthropathy is a term used to describe arthritis associated with surgical treatment of instability. It usually develops in patients who have anterior instability and undergo a surgical procedure in which the capsule is tightened excessively. This overly tightened capsule leads to a severe restriction in normal motion, especially external rotation, causing obligate translation to occur prematurely. This leads to a posterior-directed and increased joint reaction force. The result is posterior glenoid wear and articular damage.
Radiographically, capsulorraphy arthropathy form is identical to OA. However, occasional severe posterior glenoid erosions can be encountered in these cases.
Osteonecrosis
Osteonecrosis, also termed avascular necrosis, usually is subdivided into 2 categories: traumatic and nontraumatic. Traumatic osteonecrosis usually develops in patients who sustain a 3- or 4-part fracture of the humeral head that disrupts the vascular supply, mainly through the ascending branch of the anterior humeral circumflex artery to the humeral head.
In nontraumatic osteonecrosis, the disorder may be secondary to a specific disease or may be idiopathic. Commonly associated conditions include the following:
-
Smoking
-
Steroid use
-
Metabolic problems (eg, Gaucher disease, gout)
-
Hematologic disorders (eg, sickle cell disease, thalassemia)
The common pathway appears to be an impaired blood flow to the humeral head, leading to bone death.
Many different staging systems have been developed to categorize nontraumatic osteonecrosis. The Cruess classification system, which was specifically designed for humeral head osteonecrosis, is as follows:
-
Stage I: Radiographs are normal; MRI can demonstrate changes
-
Stage II: X-ray findings of sclerosis (wedged or mottled appearance) and osteopenia
-
Stage III: Radiographs demonstrate a crescent sign (subchondral fracture)
-
Stage IV: Collapse of the humeral head articular surface; loose bodies can be seen; the glenoid is not affected
-
Stage V: Arthritic changes involve the glenoid
Septic arthritis
Septic arthritis involving the shoulder is uncommon. It usually occurs in patients who are immunocompromised or debilitated.
Neuropathic arthritis
In neuropathic arthropathy, sometimes called Charcot arthropathy, the joint is destroyed secondary to loss of the trophic and protective effects of its nerve supply. This is associated with conditions such as syringomyelia, diabetes, and other causes of denervation, such as cervical spine pathology.
Patient History
History and physical examination are the most important aspects when establishing a diagnosis of glenohumeral arthritis.
Patients with significant arthritis usually present with pain and loss of motion in the shoulder. A complete history includes a description of the following:
-
Onset of symptoms
-
Aggravating or alleviating factors
-
Duration of symptoms
-
Functional difficulties
-
Timing of symptoms
-
Possible mechanisms of injury, including prior surgery
-
Other joints affected
-
Systemic diseases
-
Family history
-
Work history.
Standardized questionnaires are a valuable tool, especially for research. [5] Using them in the workup not only allows the shoulder function to be assessed reliably but also helps investigators compare results of different treatments, thus aiding in future improvements.
Findings on the history that suggest specific causes of glenohumeral arthritis include the following:
-
Osteoarthritis - Patients usually complain of pain that is slowly progressive. This pain, which is described as vague and diffuse rather than sharp and localized, often is present at rest and is exacerbated by movement and activity.
-
Inflammatory arthritides - Patients with RA involving the shoulder usually present with painful restriction of motion. These patients may have cervical spine pain and myelopathy, which can complicate the picture. The pain may be referred to the acromioclavicular (AC) joint, the subacromial bursa, or the glenohumeral joint itself.
-
Neuropathic arthritis - Patients usually suffer from a functional limitation and pain despite the denervation
-
Septic arthritis - As previously mentioned, septic arthritis usually occurs in patients who are immunocompromised or debilitated.
-
Osteonecrosis - Ask about steroid use, which is a major risk factor for osteonecrosis.
Physical Examination
A thorough examination begins with inspection of the entire upper torso for signs of muscle wasting and asymmetry. Perform a thorough cervical spine evaluation, first assessing range of motion (ROM) and tenderness, as pathology in this area can lead to referred pain in the shoulder. ROM testing consists of ranging both shoulders through flexion-extension and internal rotation/external rotation at several positions of abduction while stabilizing the scapula.
Palpation of the entire shoulder region is invaluable in arriving at the proper diagnosis. Look for areas of tenderness, defects in muscles or tendons, and masses. Strength testing consists of analyzing the power of the rotator cuff, as well as the deltoid, biceps, and scapulothoracic musculature. However, passive motion restriction often limits strength testing to rotation and abduction strength with the arm at the side. Documentation of distal vascular and neurological status also is essential.
In osteoarthritis, physical examination often reveals crepitus. In inflammatory arthritis, findings can include a warm, swollen joint and painful crepitus on ROM, as well as tenderness on palpation of the AC joint.
Plain Radiography
Standard radiographic series for evaluation of the glenohumeral joint include an anteroposterior (AP) film in the plane of the scapula and a good-quality axillary view. These films provide information on the status of the joint space, the position of the humeral head in relation to the glenoid, the presence of bony defects or deformity, the presence of osteophytes, and the quality of the bone.
A true AP view (demonstrated below) is necessary to gauge the degree of joint-space narrowing.
 The diagnosis of shoulder osteoarthritis (OA) is made on the basis of the history, physical examination, and standard radiographs. A true anteroposterior (AP) view is necessary to gauge the degree of joint space narrowing.
The diagnosis of shoulder osteoarthritis (OA) is made on the basis of the history, physical examination, and standard radiographs. A true anteroposterior (AP) view is necessary to gauge the degree of joint space narrowing.
Confirming joint-space narrowing in the shoulder is more challenging than it is in the lower extremity, where weight-bearing radiographs are used to delineate loss of joint space. Although attempts have been made to obtain stress glenohumeral radiographs, these studies have not successfully demonstrated joint-space collapse in the absence of other radiographic signs of arthritis.
An axillary radiograph is required to assess the presence of glenoid wear. If glenoid wear is seen, a computed tomography (CT) scan is the best study to evaluate the degree of osseous loss. [6] In OA, full-thickness tears of the rotator cuff are uncommon, being seen in only about 5-10% of the cases. Therefore, routine use of magnetic resonance imaging (MRI) scanning is not necessary.
Many other specialized radiographic views may be needed, depending on the findings on examination and standardized radiographs.
Osteoarthritis
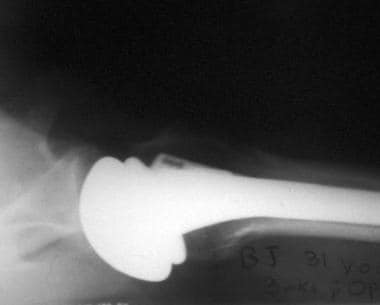
Radiographs demonstrate joint-space narrowing and osteophyte and cyst formation with subchondral sclerosis, as seen in the image below.
 Radiograph showing glenohumeral joint space narrowing and osteophyte and cyst formation with subchondral sclerosis.
Radiograph showing glenohumeral joint space narrowing and osteophyte and cyst formation with subchondral sclerosis.
Inflammatory arthritides
Plain radiographs of the shoulder with RA show findings similar to those seen in other affected joints. These findings include osteopenia, juxta-articular erosions, symmetric loss of joint space, and cystic changes. In severely affected shoulders, central glenoid erosions and humeral head elevation may be seen, as demonstrated in the image below.
 Radiograph of a severely affected joint demonstrating central glenoid erosions and humeral head elevation.
Radiograph of a severely affected joint demonstrating central glenoid erosions and humeral head elevation.
Osteonecrosis
Radiographs in patients with osteonecrosis may show resorption or, in late stages, collapse of the humeral head. (See the image below.)
 The common pathway of osteonecrosis appears to be an impaired blood flow to the humeral head, leading to bone death. Radiographs may show resorption, or in late stages, collapse of the humeral head and arthritic changes involving the glenoid as seen in this radiograph.
The common pathway of osteonecrosis appears to be an impaired blood flow to the humeral head, leading to bone death. Radiographs may show resorption, or in late stages, collapse of the humeral head and arthritic changes involving the glenoid as seen in this radiograph.
Septic arthritis
Radiographs are nonspecific but may show bone destruction in late cases.
Neuropathic arthritis
Radiographs demonstrate significant bone destruction, soft-tissue calcifications, and occasionally, joint subluxation. Therefore, neuropathic arthritis may mimic septic arthritis.
CT Shoulder Scans
A CT scan can be helpful in analyzing posterior glenoid wear when a high-quality axillary radiograph is unavailable. [7] Later stages of osteoarthritis show glenoid erosions, which usually involve the posterior glenoid and cause posterior displacement of the humeral head. CT scans can be used to assess the amount of bone loss, as seen in the image below.
CT scan and MRI, although not a standard part of the evaluation, may be helpful in preoperative planning in patients with inflammatory arthritides. CT scans are useful to gauge the amount and quality of the glenoid bone available for resurfacing or for replacement.
In addition, CT can be used to assist in planning the positioning of the glenoid component during anatomic shoulder arthroplasty. Iannotti and colleagues reported that three-dimensional CT preoperative templating proved superior to two-dimensional imaging for achieving the desired implant position within 5° of inclination or 10° of version. However, in patients undergoing three-dimensional CT templating, patient-specific instrumentation was not significantly better than standard instrumentation for enhancing accurate implant placement. [8]
MRI and Ultrasonography
MRI and ultrasonography frequently are used for diagnosis in patients with shoulder complaints. They are employed mainly to inspect the soft tissues, such as the rotator cuff. MRI may also demonstrate intra-articular changes not seen on plain films. The added benefit of the two modalities, however, is minimal in individuals with glenohumeral arthritis. [9, 10] MRI is the most sensitive diagnostic test for osteonecrosis, but cannot distinguish this condition from a bone contusion until about 8 weeks postinjury.
In patients with rheumatoid arthritis, CT scanning and MRI, although not a standard part of the evaluation of RA, may be helpful in preoperative planning.
Cell Counts and Culture
Septic arthritis
The diagnosis of septic arthritis usually is confirmed by aspiration for cell count and culture. Positive cultures or a white blood cell count of more than 75,000/µL indicate the presence of septic arthritis.
Neuropathic arthritis
Joint aspirate is negative in neuropathic arthritis.
Medical Therapy
Osteoarthritis
Nonsurgical treatment usually begins with gentle ROM exercises, nonsteroidal anti-inflammatory drugs (NSAIDs), and modification of activities or work duties that provoke the symptoms. Intra-articular injection of corticosteroids is considered in recalcitrant cases but should be used judiciously.
A report of treatment of severe glenohumeral arthritis with a spinal cord stimulator placed between the C4 and C8 nerve roots successfully reduced pain by 90% and allowed the patient to regain lost function and range of motion. [1]
Rheumatoid arthritis
Nonsurgical management is the mainstay of treatment. A well-devised treatment plan for this problem starts with a multidisciplinary team approach consisting of a rheumatologist, an orthopedic surgeon, a physical therapist, and an occupational therapist. The rheumatologist coordinates the medical management.
Medication treatment aims not only to alleviate the symptoms of RA but also to halt progression of disease. Medications used include salicylates, NSAIDs, gold salts, chloroquine, corticosteroids, and methotrexate. Methotrexate therapy has gained widespread acceptance and has shown promising results, but it has several potential side effects that require monitoring.
Physical therapy aims to reverse and prevent the stiffness seen in most shoulders affected by RA. Multiple modalities are used, including stretching programs combined with ultrasound and moist heat. Emphasis is on teaching a coordinated program that the patient can perform independently at home. In rare cases, an injection of corticosteroid may be needed to decrease the inflammation so that the patient can perform appropriate maneuvers.
Initially, physical therapy consists of a gentle stretching program and gentle isometric exercises. Physical therapy progresses to active-assisted exercises once acute inflammation has subsided. The role of the orthopedic surgeon at this stage is to monitor the ROM and the status of the joint and soft tissues.
Once the rotator cuff has failed or the articular surfaces have been destroyed, conservative therapy has failed. Recognizing when this transition has occurred is crucial in patient treatment, as prompt surgical treatment has been shown to greatly improve patient outcomes.
Surgical Therapy
Septic arthritis
Treatment consists of irrigation and debridement. Although several investigators have shown satisfactory results with serial aspiration, the criterion standard remains surgical drainage, either arthroscopically or through an open arthrotomy, with the latter yielding a slightly higher success rate. In cases with significant destruction, delayed arthroplasty after eradication of the infection can be undertaken relatively safely.
Osteoarthritis
When nonsurgical treatment is no longer effective for osteoarthritis (OA), discuss surgical options. The main surgical treatment involves joint arthroplasty. Other possible operations include debridement and synovectomy, glenoid or humeral osteotomies, arthrodesis, and resection arthroplasty. [11, 12, 13, 14]
Arthroscopic debridement and synovectomy have been shown to be effective in the early stages of OA, as long as a congruent glenoid fossa remains present. Once posterior glenoid erosion begins, this option is no longer viable. The rationale behind performing a periarticular osteotomy is to realign the joint, thus placing more force through the less-damaged portion of the joint. Although periarticular osteotomy has had limited success in the lower limb, no long-term benefit has been found when performed on the shoulder.
Resection arthroplasty, which entails removing the damaged articular surfaces and allowing the shoulder to form a fibrous joint, has a place in cases of septic arthritis and revision surgery but has not been shown to be an effective form of treatment in OA in light of results with prosthetic arthroplasty. Arthrodesis has a role in individuals with severe joint destruction and lack of function in the deltoid and rotator cuff muscles, or in patients following failed or infected joint arthroplasty. In most cases of OA, prosthetic arthroplasty is the treatment of choice.
Inflammatory arthritis
Surgical options include synovectomy and bursectomy, rotator cuff repair, and shoulder arthroplasty. [15] Synovectomy is indicated for patients with recalcitrant synovitis that is unresponsive to medical treatment and who still have a congruent joint with little or no evidence of joint destruction. This procedure can be performed through an incision (open) or arthroscopically.
The arthroscopic approach usually allows better and more complete joint visualization, as well as faster recuperation time. Debridement of the rotator cuff and labral fraying also may be accomplished.
Patient selection is the key factor in determining who will benefit from a synovectomy. Due to the lengthy attempts at conservative treatment, very few patients with RA are candidates for synovectomy and bursectomy. In general, patients may be better served by earlier intervention by surgeons.
Arthroplasty is the most commonly performed procedure for the shoulder with inflammatory arthritis. Once a surgeon decides to perform shoulder arthroplasty, some technical areas must be addressed.
Rotator cuff damage
Rotator cuff repair has been shown to give satisfactory results in terms of comfort and function in the subset of patients with RA who have reparable cuff problems and little joint destruction. Long-term outcomes of these patients compared with patients without RA are not available.
Glenohumeral Arthrodesis
This surgical technique involves creating a bony fusion between the humeral head and the glenoid, as well as the humeral head and acromion. Like resection arthroplasty (described below), this technique has fallen out of favor except for a very few indications. These indications include salvage attempts after severe septic arthritis, arthritis or bone loss with a superimposed rotator cuff and deltoid deficiency, refractory shoulder instability, and failed joint arthroplasty with severe bone loss.
Many surgical techniques have been advocated, including intra-articular and extra-articular fusions using a variety of internal and external fixation devices. Positioning the arm has been a subject of debate, but most surgeons advocate placing the arm in 20-40° of abduction, 20-30° of flexion, and 25-40° of internal rotation.
Fusion rates remain fairly good, with a very low rate of surgical complications. Patient satisfaction is approximately 80%. Complications include infection, nerve injury, neck and scapular pain, and inability to perform the activities of daily living that require external rotation.
Shoulder Arthroplasty
The primary indication for shoulder arthroplasty is pain that is no longer controlled with conservative means. Improvement in function should be considered a bonus of the surgery rather than an indication.
Although the decision to perform arthroplasty should be individualized to each patient's case, several general indications should be met. For example, the patient should have a severe disability in the affected shoulder, with the disability related to the loss of articular competency.
In addition, conservative measures should have been exhausted, and the shoulder itself should be amenable to surgery, with sufficient bone stock remaining to warrant placement of a prosthesis
Medically, the patient should be able to tolerate the operation with acceptable risk and should understand the procedure, including risks and limitations, as well as the rehabilitation required.
Indications for arthroplasty
Specific shoulder-related indications for total shoulder replacement are as follows:
-
Most cases of OA, particularly if there is eccentric glenoid wear
-
Inflammatory arthritis with an intact rotator cuff and minimal central glenoid erosion
-
Capsulorraphy arthropathy
Indications for hemiarthroplasty
Hemiarthroplasty, which is far less technically demanding than total shoulder replacement, is considered in cases of the following:
-
Severe articular cartilage wear with concomitant roughness on the humeral side, with little glenoid wear
-
Cuff tear arthropathy or glenohumeral arthritis with a concomitant rotator cuff tear and superiorly translated humeral head
-
Inflammatory arthritis and severe central glenoid wear to such a degree that the remaining glenoid bone stock would be insufficient to hold a glenoid component
-
Patients who are young and have heavy demands (relative indication) [16]
Specific shoulder-related indications for hemiarthroplasty are as follows:
-
OA with absolutely no eccentric glenoid wear
-
Inflammatory arthritis with severe central glenoid erosion
-
Avascular necrosis (AVN)
-
Cuff tear arthropathy [16]
-
Revision for loose glenoid component
Goals and long-term risk of shoulder replacement
The goals of arthroplasty are to restore glenohumeral motion, strength, stability, and smoothness while providing excellent pain relief. Total arthroplasty is performed in patients with severe wear of the humeral head and glenoid surfaces. Follow-up studies have shown some overlap in indications. Pain relief and postoperative ROM seem to be better and more consistent in cases of total arthroplasty.
The long-term risk of glenoid component loosening with total shoulder replacement must be weighed against the risk of progressive glenoid wear with a hemiarthroplasty. Currently, data to compare these variables accurately are unavailable.
In a study of 5279 patients 30 to 50 years old with severe end-stage glenohumeral arthritis refractory to conservative management, hemiarthroplasty as the initial treatment resulted in 59,574 patient years of satisfactory or excellent results (11.29 per patient) and average quality-adjusted life-years (QALYs) gained of 6.55, whereas total shoulder arthroplasty (TSA) resulted in 85,969 patient years of satisfactory or excellent results (16.29 per patient) and average QALYs gained of 7.96. Researchers further concluded that TSA for this population, instead of hemiarthroplasty, is more cost-effective and result in a substantial reduction in the number of revision procedures. [17]
Absolute contraindications to shoulder replacement
Absolute contraindications to shoulder arthroplasty are the following:
-
Active sepsis
-
Functional loss of both the deltoid and the rotator cuff (eg, irreparable rotator cuff tear in the presence of an axillary nerve palsy)
Relative contraindications to shoulder replacement
Neuropathic joint (Charcot arthropathy) is one relative contraindication to arthroplasty. Although an arthroplasty may be performed and may provide some pain relief (if present), there is an increased rate of instability and loosening. Treatment instead consists of correcting the underlying condition, if possible
Loss of the stabilizing function of the coracoacromial arch is another relative contraindication. If a patient has superior instability from an irreparable rotator cuff tear combined with prior acromial resection, arthroplasty probably will offer little help.
Alcohol abuse and seizure disorder are risk factors as well, with the chance of shoulder instability occurring in individuals with either condition being abnormally high.
Total shoulder replacement versus hemiarthroplasty in osteoarthritis
Osteoarthritis is by far the most common indication for total shoulder replacement, [18] A systematic review and meta-analysis by Bryant and colleagues that included a total of 112 patients found that at a minimum of 2 years of follow-up, total shoulder arthroplasty provided better functional outcome than hemiarthroplasty for patients with osteoarthritis of the shoulder. [19]
Similarly, a meta-analysis by Singh and colleagues found that in patients with osteoarthritis, total shoulder arthroplasty seems to provide superior shoulder function compared with hemiarthroplasty, but the two procedures demonstrate no statistically significant difference with respect to other clinical outcomes (eg, pain scores, quality of life). [20]
In a single-institution review by Levine and colleagues of 31 shoulder hemiarthoplasties in 30 patients with osteoarthritis, only 25% of patients were satisfied with their outcome at an average of 17 years after the operation. [21] Outcomes were better in patients with concentric glenoid wear and primary osteoarthritis than in those with eccentric glenoid wear and secondary osteoarthritis.
Total shoulder replacement versus hemiarthroplasty in rheumatoid arthritis
Adding a glenoid component usually is based on several factors, including the integrity of the rotator cuff, the amount of glenoid bone stock to support a glenoid component, and the amount of space available to insert a glenoid component without greatly overstuffing the joint.
If the rotator cuff is torn or ineffective and the humeral head is translated proximally, thus articulating with the coracoacromial arch, a hemiarthroplasty should be performed. The use of hemiarthroplasty maintains this balance point, and studies have shown surprisingly good functional results.
For patients who have maintained glenoid concavity and a concentric glenohumeral position, either hemiarthroplasty or total shoulder arthroplasty are reasonable options. In this patient population, functional outcomes for both of these procedures are excellent, with a trend toward improved pain relief in the total shoulder group. [22, 23, 24, 25, 26, 27, 28] In patients with posterior glenoid wear, glenoid resurfacing is necessary.
For the patient with significant posterior glenoid wear and an age younger than 50 years, consider humeral hemiarthroplasty combined with glenoid reaming and possible nonprosthetic resurfacing, such as fascial arthroplasty. [29]
In patients with so much medial glenoid erosion that a glenoid component cannot be adequately supported, a hemiarthroplasty should be performed. Circumferential contraction of the capsule and supporting soft tissue that leads to decreased joint volume is a relative contraindication to placing a glenoid component.
If hemiarthroplasty is to be performed, the surgical technique should be modified. For example, the coracoacromial arch should be kept intact to help constrain the prosthetic head. The degree of pain relief may be greater with total shoulder arthroplasty. Moreover, by removing all of the remaining glenoid chondral surface, the precipitating cause of synovitis is, theoretically, eliminated.
Cemented versus uncemented arthroplasty in rheumatoid arthritis
Studies have demonstrated progressive loosening of uncemented components in nearly 50% of patients with RA, compared with almost nonexistent loosening in cemented prostheses. [30] However, these studies were performed mostly with a component designed for cemented fixation. How current uncemented designs fare in the rheumatoid population is unknown.
In a series of patients with primary glenohumeral osteoarthritis younger than 60 years old, the survival of a cemented polyethylene glenoid component was three times higher than that of a cementless metal-backed glenoid component (22% vs 70%) ten years after surgery. Glenoid loosening or failure was the indication for revision in the polyethylene group, whereas polyethylene wear with metal-on-metal contact, instability, and insufficiency of the rotator cuff were the indications for revision in the metal-backed group. [31]
Resection arthroplasty
Surgical resection of the humeral head, though more common before the advent of prostheses, still is part of a surgeon's armamentarium. The procedure may be indicated in the following settings:
-
Debilitated patients with severe fractures not amenable to placement of prosthesis
-
Patients with severe septic arthritis and concomitant osteomyelitis of the glenoid or humeral head
-
Patients with a failed arthroplasty with osseous and soft-tissue deficiencies.
In the third type of case, above, several authors have reported modest outcomes, with variable pain relief.
Intraoperative Details for Arthroplasty
A deltopectoral approach is used. The cephalic vein is kept laterally, while the interval is developed. The clavipectoral fascia then is incised up to, but not through, the coracoacromial ligament.
The subscapularis muscle usually is incised near its insertion into the lesser tuberosity, preserving its length. Alternatively a lesser tuberosity osteotomy may be performed allowing reflection of the subscapularis without violating the tendon substance. The underlying anterior capsule can be incised with the subscapularis muscle or incised separately after being dissected free from the overlying muscle and tendon. The subscapularis muscle then should be completely mobilized 360° to allow it to move freely from the underlying capsule.
Humeral preparation is then completed, with the precise steps depending on the implant system chosen. Initially, circumferential osteophytes are removed from the humeral head. The humeral osteotomy is made at the level of the rotator cuff insertion, either free hand or with a template jig.
The version of the cut is either set to match the patient's own version or set at a predetermined normal of approximately 30°. The ideal humeral cut should allow the humeral implant to be placed in the anatomic position, replacing only the amount resected. The angle of the cut should match that of the prosthesis.
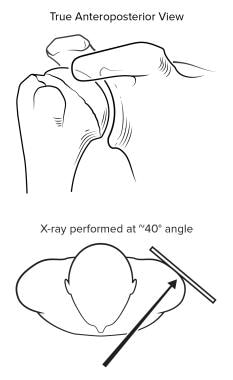
For uncemented systems, basing the humeral osteotomy off of an intramedullary rod helps to orient the component correctly to the orthopedic axis of the humeral shaft. (See the image below.)
 For uncemented arthroplasty systems, basing the humeral osteotomy off of an intramedullary rod helps to orient the component correctly to the orthopedic axis of the humeral shaft.
For uncemented arthroplasty systems, basing the humeral osteotomy off of an intramedullary rod helps to orient the component correctly to the orthopedic axis of the humeral shaft.
Once the trial component is placed, the surgeon can determine whether a centrally placed humeral head component covers the surface of the cut (ie, the normal head is positioned centrally on the humeral orthopedic axis) or whether an eccentrically placed head is required. (See the image below.)
 Once the trial component is placed during an arthroplasty procedure, the surgeon can determine if a centrally placed humeral head component will cover the surface of the cut (ie, the normal head is centrally positioned on the humeral orthopedic axis), or if an eccentrically placed head will be required.
Once the trial component is placed during an arthroplasty procedure, the surgeon can determine if a centrally placed humeral head component will cover the surface of the cut (ie, the normal head is centrally positioned on the humeral orthopedic axis), or if an eccentrically placed head will be required.
The glenoid is approached next. Proper exposure is of utmost importance. Defining the centerline and the centering point on the glenoid face is the first step. The centering point is the midpoint of the glenoid face. Once this spot is found, the glenoid jig is placed, and the glenoid is prepared according to the implant technique manual. The orientation of the glenoid face is normalized using an appropriately oriented reamer. The goals of reaming are to reorient the glenoid face, to remove enough glenoid bone to fit a component, and to create a complete circumferential backing for the glenoid component.
The trial components then are inserted, and the shoulder is reduced and brought through a ROM. Joint volume, proper version, and integrity and tensioning of the rotator cuff are assessed.
Properly placed components allow 70° of internal rotation with the arm at 90° of abduction, 15 mm of posterior translation with a spring-back of the head upon removal of the posterior directed force, and at least 40° of external rotation with approximated subscapularis closure. Most important, the replacement should reproduce the normal tuberosity offset and head height, and should look like a normal anatomic glenohumeral joint (see the image below).
 A glenohumeral prosthesis should reproduce the normal tuberosity offset and head height and should look like a normal anatomic glenohumeral joint.
A glenohumeral prosthesis should reproduce the normal tuberosity offset and head height and should look like a normal anatomic glenohumeral joint.
Modular implant designs allow greater latitude in the preparation phase. The components then are inserted, and the subscapularis muscle is reattached to the humeral osteotomy through drill holes, thus lengthening the subscapularis and further providing external rotation.
When intraoperative difficulties with the glenoid component or instability arise during a total shoulder arthroplasty, changing to a reverse shoulder arthroplasty may be considered. Steen et al studied 24 consecutive patients with glenohumeral osteoarthritis who were converted intraoperatively to a reverse shoulder arthroplasty because of improper seating of the glenoid trial or persistent posterior subluxation and found that outcomes were similar, compared with 96 patients undergoing total shoulder arthroplasty. Radiographic glenoid loosening developed in five of the total shoulder arthroplasty patients, but in none of the reverse shoulder arthroplasty patients. Costs were higher with reverse shoulder arthroplasty, mainly due to implant cost. [32, 33]
Postoperative Care
Surgical rehabilitation begins intraoperatively. Use of interscalene anesthesia facilitates immediate postoperative rehabilitation. Proper component positioning and soft-tissue release are essential for adequate postoperative motion. Functional ROM must be achieved prior to leaving the operating room.
The surgeon must not rely on the postoperative regimen to stretch out the shoulder; rather, the postoperative program simply maintains the intraoperative gains. Finally, prior to closure, the surgeon should assess the maximum external rotation capable prior to tension on the subscapularis repair, as this degree is used to set the postoperative limit.
The goals of the postoperative period include the return of pain-free shoulder motion and the prevention of complications. Patients usually stay in the hospital 1-3 days. Continuous passive motion has been shown to be of use, although not in comparative studies. Passive ROM (PROM) usually is started either in the recovery room or on the first postoperative day.
Forward elevation and external rotation are the mainstays in most rehabilitation plans. These exercises usually are performed in the supine position using the nonoperative arm to execute the desired arc of motion, termed self-passive. The goals before discharge are 140° of forward elevation and 40° of external rotation, depending upon the subscapularis repair.
In addition to ROM exercises, isometric deltoid strengthening is performed. Active nonisometric motion usually is restricted for the first 6-8 weeks to prevent surgical dehiscence of the tendinous repair. Patients may perform light activities of daily living, and aerobic conditioning is encouraged. The only specific restriction is internal rotation against resistance, such as closing a heavy door.
After the first 6 weeks, gentle rotator cuff strengthening may be added to the regimen. Internal rotation stretching usually is unnecessary, as most patients have preoperative stretching of the posterior capsule secondary to posterior subluxation. At 3 months postsurgery, patients may return to swimming, golf, tennis, and all other noncontact sports.
For patient education information, see eMedicineHealth's patient education article Osteoarthritis.
Surgical Outcomes
With proper patient selection, the results for prosthetic surgery are excellent. Patient satisfaction rates are 86-100%. For pain relief, most studies show over 90% favorable outcomes. Functional outcomes have lagged behind pain relief but still are improved in most patients.
Several studies have shown that earlier intervention and arthroplasty treatment lead to better functional and symptomatic outcomes, thus reinforcing the notion that surgical treatment should not be delayed when conservative treatment has failed.
Long-term outcomes (8-17 years) of total shoulder arthroplasty in 21 middle-aged patients with osteoarthritis were assessed. The Constant-Murley score (CS) with its subgroups and subjective satisfaction were measured. The mean CS increased from 23.3 (10 to 45) pre-operatively to 56.5 (26 to 81; p < 0.0001), but decreased from 62.8 (38 to 93) to 56.5 (26 to 81) between medium- and long-term follow-up (p = 0.01). Radiological signs of implant loosening were also analysed. The mean radiolucent line score for the glenoid components increased from 1.8 (0 to 6) to 8.2 (2 to 18) between medium- and long-term follow-up (p < 0.001). [34]
Surgical Complications
Instability
Complications of shoulder arthroplasty fortunately are rare. The most common complication of shoulder arthroplasty is instability, as seen in the radiograph below, with a reported rate of 2-5%.
Several factors are related to the development of instability, including cuff integrity, glenoid component orientation, and maintenance of the stabilizing function of the coracoacromial arch. Instability usually is a technical error involving improper implant sizing, version, or soft-tissue balancing.
Treatment of instability is based on the underlying cause. A common pattern is posterior instability after hemiarthroplasty for OA. Usually, the underlying cause is unrecognized posterior glenoid wear, and treatment requires glenoid replacement. (See the image below.)
 A common pattern of instability is posterior instability after hemiarthroplasty for osteoarthritis. Usually, the underlying cause is unrecognized posterior glenoid wear, and treatment requires glenoid replacement.
A common pattern of instability is posterior instability after hemiarthroplasty for osteoarthritis. Usually, the underlying cause is unrecognized posterior glenoid wear, and treatment requires glenoid replacement.
Infection
Infection (see the image below) is a dreaded problem. Fortunately, it occurs rarely (in 0.1-1% of shoulder arthroplasty cases), developing less often in shoulder arthroplasty than it does in other major joint replacements. The shoulder seems to be conferred with some protection, probably owing to its abundant blood supply.
 If infection occurs following shoulder arthroplasty, prompt surgical treatment must be undertaken. Placing an antibiotic impregnated spacer (as shown below) to maintain soft-tissue tension is preferable if humeral bone stock is adequate.
If infection occurs following shoulder arthroplasty, prompt surgical treatment must be undertaken. Placing an antibiotic impregnated spacer (as shown below) to maintain soft-tissue tension is preferable if humeral bone stock is adequate.
However, patients with inflammatory arthritides are at a higher risk than are those with degenerative arthritis, because of the systemic nature of the disease, immunosuppression, steroid dependence, and poor tissue healing.
When an infection occurs, prompt surgical treatment must be undertaken. Early infections with a sensitive organism can be treated with aggressive irrigation and debridement, and usually with prolonged intravenous antibiotic treatment. In cases of a resistant organism, or subacute or chronic infections, debridement with prosthetic removal is required.
Placing an antibiotic-impregnated spacer to maintain soft-tissue tension is preferable if humeral bone stock is adequate. The rules of prosthetic reimplantation are similar to those for hip arthroplasty.
Glenoid loosening
Another common complication associated with total shoulder arthroplasty is glenoid loosening. It has been reported with a frequency of approximately 1% per year.
A strong correlation exists between glenoid loosening and the presence of a full-thickness rotator cuff tear.
Matsen and colleagues coined the term "rocking horse glenoid" to describe the effect of the superior shear force on the glenoid component that accompanies the lack of an effective cuff mechanism. [35] Therefore, glenoid component implantation is contraindicated in the presence of a full-thickness rotator cuff tear.
Rotator cuff deficiency
A deficient rotator cuff may tear, which can lead to , which can lead to superior migration of the humeral head. See the image below.
 Radiograph demonstrating superior migration of the humeral component after total shoulder arthroplasty consistent with the development of a massive rotator cuff tear.
Radiograph demonstrating superior migration of the humeral component after total shoulder arthroplasty consistent with the development of a massive rotator cuff tear.
Early in the postoperative period, subscapularis problems are a major concern. The subscapularis may tear in the early postoperative period. Alternatively, the subscapular nerves may be injured during subscapularis mobilization. Almost all patients who undergo shoulder arthroplasty have weakness of subscapularis function, defined by lack of lumbar lift or abdominal push strength, for the first few months after arthroplasty.
The defining physical examination finding for a subscapularis rupture is a sudden, dramatic increase in passive external rotation. Imaging is complicated by the presence of a prosthetic component, but ultrasonography may be helpful in equivocal cases. Late cuff tearing usually involves the supraspinatus and is related primarily to superior or varus positioning of the humeral component or oversizing of the humeral prosthesis with resultant joint stuffing.
Other surgical complications
Other complications of shoulder replacement surgery include fracture, thromboembolism, and heterotopic bone formation. Fractures usually occur on the humeral side from overzealous reaming or during dislocation secondary to inadequate soft-tissue release. Heterotopic ossification is common but rarely is clinically significant.
Future Directions in Surgery
Several possibilities exist for the future management of the arthritic shoulder. It is hoped that the techniques of cartilage transplantation currently being perfected in the knee will be used more frequently in the glenohumeral joint. Future enhancements in glenoid replacement likely will be made, including improved component design, better materials, and improved fixation methods.
Finally, surgeons will be experimenting more with nonprosthetic arthroplasty, particularly on the glenoid side. Hemiarthroplasty combined with fascial resurfacing of the glenoid has been used for treating a few young patients with osteoarthritis. [36, 37] These efforts likely will continue.
-
The diagnosis of shoulder osteoarthritis (OA) is made on the basis of the history, physical examination, and standard radiographs. A true anteroposterior (AP) view is necessary to gauge the degree of joint space narrowing.
-
Radiograph showing glenohumeral joint space narrowing and osteophyte and cyst formation with subchondral sclerosis.
-
CT scan can be used to assess the amount of bone loss around the glenohumeral joint.
-
Radiograph of a severely affected joint demonstrating central glenoid erosions and humeral head elevation.
-
Radiograph demonstrating superior migration of the humeral head. This is seen in the setting of a long-standing massive rotator cuff tear where the normal function of the rotator cuff acting as a humeral head depressor has been lost.
-
The common pathway of osteonecrosis appears to be an impaired blood flow to the humeral head, leading to bone death. Radiographs may show resorption, or in late stages, collapse of the humeral head and arthritic changes involving the glenoid as seen in this radiograph.
-
For uncemented arthroplasty systems, basing the humeral osteotomy off of an intramedullary rod helps to orient the component correctly to the orthopedic axis of the humeral shaft.
-
Once the trial component is placed during an arthroplasty procedure, the surgeon can determine if a centrally placed humeral head component will cover the surface of the cut (ie, the normal head is centrally positioned on the humeral orthopedic axis), or if an eccentrically placed head will be required.
-
A glenohumeral prosthesis should reproduce the normal tuberosity offset and head height and should look like a normal anatomic glenohumeral joint.
-
Radiograph demonstrating anterior instability after a total shoulder arthroplasty
-
A common pattern of instability is posterior instability after hemiarthroplasty for osteoarthritis. Usually, the underlying cause is unrecognized posterior glenoid wear, and treatment requires glenoid replacement.
-
If infection occurs following shoulder arthroplasty, prompt surgical treatment must be undertaken. Placing an antibiotic impregnated spacer (as shown below) to maintain soft-tissue tension is preferable if humeral bone stock is adequate.
-
Radiograph demonstrating superior migration of the humeral component after total shoulder arthroplasty consistent with the development of a massive rotator cuff tear.
Tables
What would you like to print?
- Practice Essentials
- Shoulder Anatomy
- Shoulder Arthritides
- Patient History
- Physical Examination
- Plain Radiography
- CT Shoulder Scans
- MRI and Ultrasonography
- Cell Counts and Culture
- Medical Therapy
- Surgical Therapy
- Glenohumeral Arthrodesis
- Shoulder Arthroplasty
- Intraoperative Details for Arthroplasty
- Postoperative Care
- Surgical Outcomes
- Surgical Complications
- Future Directions in Surgery
- Show All
- Media Gallery
- References











