Background
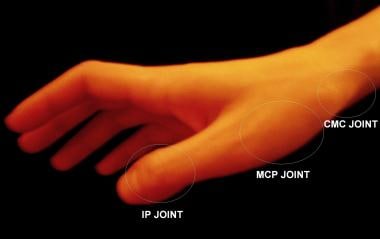
Despite the inherent stability of the joints of the thumb, the vulnerable anatomic position of the first phalanx often subjects the joints to mechanical strain that leads to subluxation or dislocation of the metacarpophalangeal (MCP) and interphalangeal (IP) joints. (See the image below.) These and other thumb injuries are particularly common in athletes. [1]
The MCP joint of the thumb is a condyloid joint that has a structurally stronger capsular ligament apparatus than the other four MCP joints of the hand do. [2] Most thumb MCP dislocations are dorsal. [3] They are caused by a longitudinal and dorsal stress along the axis of the digit that hyperextends the thumb and tears the volar plate of the joint. An example of this mechanism is a fall onto an outstretched hand (FOOSH) with an impact to the tip of an extended thumb.
Volar dislocation of the MCP joint of the thumb is comparatively rare and is associated with tears of both dorsal capsule ligaments and the extensor pollicis brevis (EPB). [4] For this reason, anterior dislocations are often treated with surgical repair of the torn structures, [5] and closed reduction is rarely achieved with adequate postreduction stability.
Plain film radiography is the definitive diagnostic modality for joint dislocations of the thumb, serving both to describe the geography of the dislocation and to rule out the possibility of coexisting fractures.
Intra-articular fractures should be excluded by means of radiology before an attempt is made to reduce a joint in the thumb. These fractures include the Bennett fracture or oblique fracture through the base of the first metacarpal with dislocation of the radial portion of the articular surface. [6, 7] The Rolando fracture is similar to the Bennett fracture, except that the fracture at the base of the metacarpal is comminuted with similar dislocation of the fragments.
Dislocation of the IP joint occurs to a much lesser extent than dislocation of the MCP joint does. These injuries are most commonly dorsal and are often associated with disruption of the overlying skin and soft tissues.
Although rare cases of multiple simultaneous thumb joint dislocations, including the IP, MCP, and proximal carpometacarpal (CMC) or trapeziometacarpal (TMC) joints, have been reported in the literature, most thumb dislocations involve only a single joint. [8, 9, 10, 11, 12, 13, 14] The existence of multiple thumb joint dislocation injury underscores the necessity of careful radiographic analysis before reduction attempts are made. [15]
Indications
Indications for reduction of a thumb dislocation include the following:
-
Radiographic evidence of dorsal dislocation of the first MCP or IP joint with no simultaneous radiographic evidence of intra-articular fracture of the carpals, the first metacarpal, or the first proximal or distal phalanx
-
Clinical history and examination consistent with acute dislocation of the MCP or IP joint of the thumb with significant neurovascular deficits on examination that began at any time after the injury; in this emergency scenario, reduction should not be delayed to acquire radiologic assessment
Contraindications
Absolute contraindications for reduction of a thumb dislocation include the following:
-
Simultaneous intra-articular fracture of the carpals, the first metacarpal, or the first proximal or distal phalanx
-
Epiphyseal plate injury of the carpals, the first metacarpal, or the first proximal or distal phalanx
Relative contraindications include the following:
-
Persistence of nonossified physeal plate in a dislocation that does not reduce with minimal force
-
Volar dislocations of the MCP or IP joint of the first digit [16]
-
Anatomic locations of joints of thumb.
-
Position of hyperextension used for reduction of dorsal interphalangeal (IP) joint dislocation.
-
Position of hyperextension used for reduction of dorsal metacarpophalangeal (MCP) joint dislocation.
-
Hand position used for testing if laxity is present with valgus strain of metacarpophalangeal (MCP) joint. Such laxity suggests presence of ulnar collateral ligament (UCL) tear and indicates possible existence of Stener lesion.