Practice Essentials
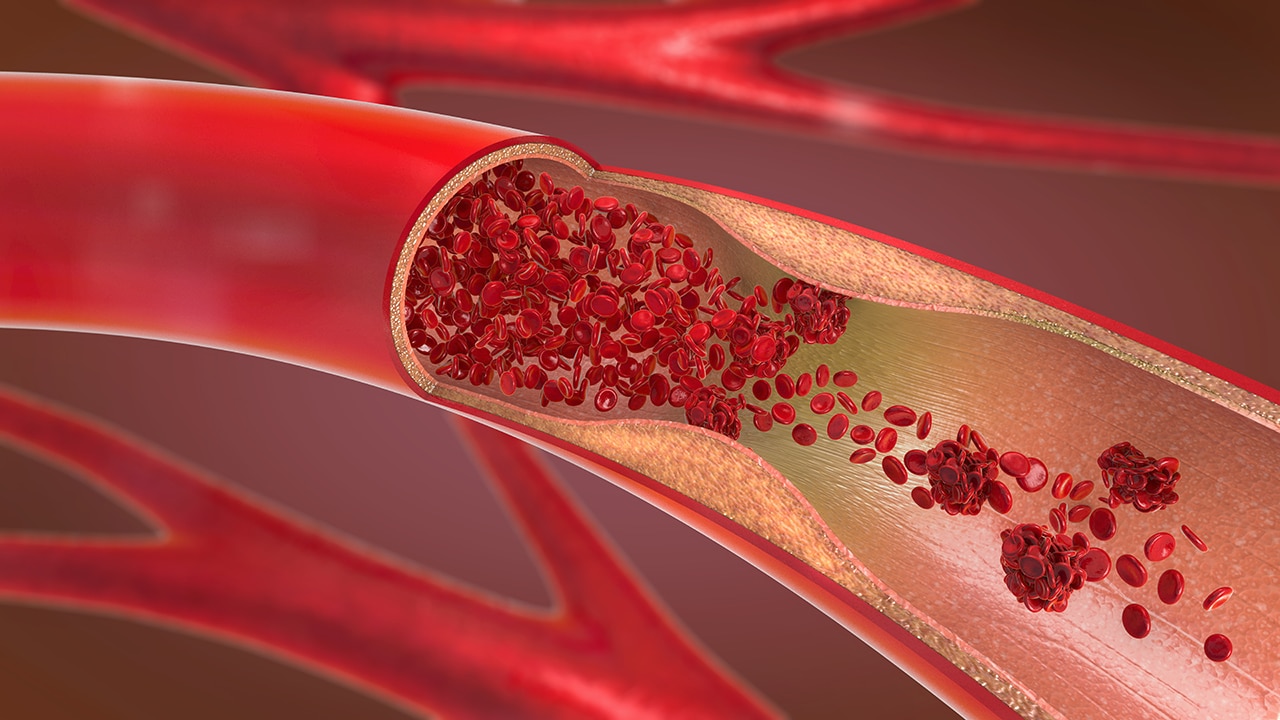
Venous thromboembolism (VTE) is a multifactorial disease driven by environmental/acquired risk factors such as age, obesity, oral contraceptives, and immobility, as well as inherited risk factors such as genetic polymorphisms. [1, 2, 3] VTE causes formation of blood clots, primarily of the deep veins. In the United States, it affects 300,000 to 600,000 individuals each year, proving fatal in over 100,000. The incidence is highest in people older than 80 years, with highest incidences reported in individuals of European or African ancestry. [4] There have been a variety of investigations into the genetic determinants of VTE, ranging from candidate gene studies to genome-wide association studies. These investigations have led to the discovery of genetic variants that result either in an excess of a prothrombotic factor or a deficiency in an antithrombotic factor. Factor V Leiden is the most common and well-studied genetic cause of VTE, with the factor II c.*97G>A (formerly referred to as prothrombin 20210G>A) gene mutation and deficiencies in protein S, protein C, and antithrombin accounting for most of the remaining cases. [5, 6, 7, 8, 9, 10, 11, 12, 13]
Genetic testing commonly includes levels of antithrombin, protein C, or protein S to identify a deficiency, as well as factor V Leiden and factor G20210A, or factor II c.*97G>A. [5]
Several single-nucleotide polymorphisms (SNPs) in candidate genes have been associated with disease risk, including F5 rs6025, F2 rs1799963, FGG rs2066865, and ABO genetic variants. [3, 14]
There are 6 introns and 7 exons in the gene encoding antithrombin (SERPINC1). Antithrombin deficiency leads to the highest risk of venous thromboembolism among deficiencies of natural anticoagulants. There are reports of more than 200 mutations in SERPINC1 that cause antithrombin deficiency. Antithrombin Rybnik is a point mutation associated with quantitative antithrombin deficiency. [15]
Genetic variants in the ABO blood-type loci have also been associated with an increased risk of VTE. Specifically, persons with blood type O or A2 have a lower risk of developing VTE than do individuals with other blood types. [16] This difference is thought to result from the presence of higher levels of von Willebrand factor and factor VIII—2 known risk factors for VTE—in persons with non-O blood types. [17, 18]
An increased VTE risk has also been associated with variants near CYP4V2 [19] in the factor XI gene [20] that increase factor XI levels.
These associations highlight the critical balance that prothrombotic and antithrombotic factors must strike to maintain hemostasis and prevent pathologic thrombosis.
Two studies have identified a genetic variant in GP6, a gene that encodes the platelet collagen receptor, that confers an increased risk of VTE. [16, 19] This discovery implicates a platelet-specific factor in the pathogenesis of VTE.
Genome-wide association studies (GWASs) have discovered a number of VTE-associated loci. The GWAS-discovered risk variants are weak risk factors for VTE but are prevalent in the population. [21, 22, 23]
Lindstrom et al conducted a meta-analysis of GWAS data for VTE of 18 studies with 30,234 VTE patients. Eleven newly associated genetic loci (C1orf198, PLEK, OSMR-AS1, NUGGC/SCARA5, GRK5, MPHOSPH9, ARID4A, PLCG2, SMG6, EIF5A, and STX10) were identified. The strongest genetic risk factors for VTE were found to be related to coagulation or the anticoagulation system. This study added several loci involved directly or indirectly in platelet biology. [21]
Risk conferred by genetic variants may be magnified when combined with acquired risk factors. For example, risk of VTE in carriers of the factor V Leiden or prothrombin gene mutation is increased by use of oral contraceptives, [24, 25] hormone replacement therapy, [26] and smoking. [27]
Clinical Implications
Widespread testing for mutations that might increase the risk of VTE is not warranted. However, in patients presenting with a VTE, testing should be considered if the following factors are present:
-
Age less than 50 years
-
Thrombosis at unusual sites
-
Recurrent VTE
-
Strong family history of thrombotic disease
Susceptibility to venous thromboembolism is very complex. Pathobiology of VTE involves both genetic and acquired factors. Patients who have had VTE have a genetic predisposition due to molecular abnormalities in the components of the coagulation cascade. Common genetic abnormalities, particularly among whites, include factor V Leiden and prothrombin gene 20210A mutations. Additionally, some abnormalities are found in gene loci antithrombin, protein C, and protein S. [28]
Although carriers of the factor V Leiden or prothrombin gene mutations may have a higher risk of recurrent VTE, the magnitude is likely small, [29] and it is unclear whether genetic testing at the time of a first VTE improves outcomes. [30, 31] The importance of obtaining a family history, a simple and frequently underutilized tool available to all clinicians, has been stressed by the Office of Genomics and Disease Prevention at the Centers for Disease Control and Prevention (CDC). [32]
Although the presence of a factor V Leiden mutation is not an absolute contraindication for oral contraceptive use, because of the high risk for VTE conferred by the combination, women who are heterozygous for factor V Leiden should be discouraged from the use of oral contraceptives. Similarly women with a personal or family history of unprovoked VTE at a young age who are considering oral contraceptive use can benefit from genetic testing and counseling. [6]